The trend towards collaboration within general practice continues apace. As my colleague Stephanie Kumpunen explained in her recent blog, our recent surveys of GPs and CCGs give reason to be cautiously optimistic that scaled-up general practice is beginning to make some progress towards the goals it’s intended to deliver.
But general practice does not work in isolation and its future is inevitably tied up in the wider system that is undergoing widespread change.
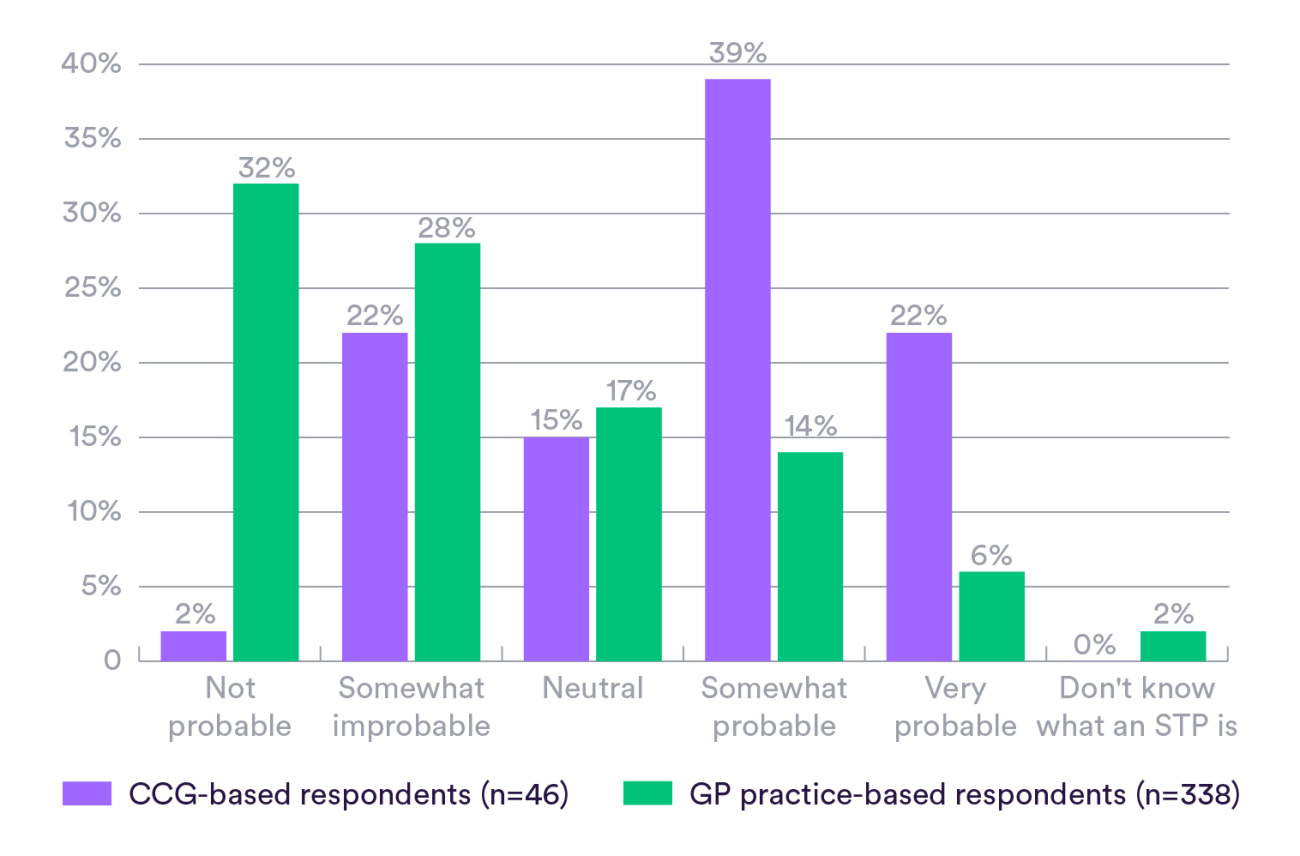
We asked more than 560 GPs how they felt about their local sustainability and transformation partnerships (STPs) and what they felt the future held for their practices. The responses provide interesting reading but also some concerning messages.
Influencing change
Intended as the first step on the path to integrated place-based systems, STPs herald potentially significant changes to service delivery and system structures. They set out ambitious plans to transform the delivery of care by shifting care out of hospital and into the community. Many of these plans rely heavily on robust and sustainable general practice.
If there’s one thing we’ve learnt over the years of studying change in health care systems, it’s that for service transformation to be sustained, leaders need to win the hearts and minds of the frontline staff who will actually be delivering it. STP plans are no exception. In fact, as STPs are not established as new statutory bodies, they have no direct or contractual ‘powers’ over members. Instead, they rely upon good relationships, common goals and shared values.
Engaging all members in the vision is therefore crucial. This is where our survey identified some concerning messages.
Of the GPs who responded to our survey, over half said their practice or group of practices had not been influential at all in the development of their local STP. Fewer than one-fifth of respondents felt they had been somewhat or very influential.
It’s not clear from our survey whether GPs chose not to influence STPs or felt unable to, but either way this makes for worrying reading. Is it likely that change will be delivered if a key player feels they have little or no influence in decisions?
Perhaps having influence isn’t so important if GPs believe in the vision but it’s not clear that they do.
We found that 60 per cent of GPs think it’s unlikely their local STP vision will translate into meaningful change on the ground for primary care. Interestingly, the same proportion of CCG respondents said the opposite – that STPs will deliver meaningful change for primary care.
This mismatch in views suggests there is work to be done in aligning plans and expectations about what role primary care can and will play in future.
General practice on the sidelines or taking centre stage?
Our survey results also raise a more fundamental question about the role general practice sees for itself in a future system. GPs expressed enthusiasm for general practice taking on contracts for selected community services and (albeit a smaller number of respondents) for some hospital services.
However, over half of GPs indicated an unwillingness to move away from their General Medical Services (GMS) or Personal Medical Services (PMS) contract to become an associate practice in a local collaborative arrangement, such as a multispecialty community provider (MCP) or a primary and acute care system (PACS). A further fifth didn’t know if they would be willing or felt neutral about it.
Respondents had concerns that entering into such a contract would spell the loss of their autonomy and decision-making powers. A large number simply said they didn’t know what it would mean for them and, without further clarification, they would not be willing to shift.
Given the lack of buy-in to the overall STP vision, it’s perhaps not surprising that GPs feel reluctant to take a leap into the contractual unknown, but it does raise questions whether general practice is prepared to fully engage, and take centre stage, in system change.
Making transformation sustainable
Of course, we should caveat our findings – this was a modest sample of GPs and we can’t discount the possibility of bias. But the messages are still concerning and policy-makers need to take note.
If STPs are going to be successful in not just transforming services but also sustaining change, our survey suggests that a number of things need to happen.
First, there is a need for concerted effort to ensure all partners in an STP area feel engaged. We would urge STP leaders to learn the lessons of the past and to take the time to understand why GPs have not felt influential, and then create a vision into which all providers in a locality can buy.
Second, STP leaders need to support GP collaborations to become the well-functioning and robust foundations that are required to deliver the ambitious plans they have created. Without strong general practice, it’s unlikely that the aims set out in STP plans will be deliverable.
Last, GP leaders need to make sure that, as well as building their organisations, they are simultaneously outward looking and engaged in the wider system. Time and work pressures will always be confounding factors but this is a critical moment for general practice to decide what role it wishes to play in a future system.
Suggested citation
Curry, N. (2017) "Transforming and sustaining change: What’s the role of general practice?" Nuffield Trust comment www.nuffieldtrust.org.uk/news-item/transforming-and-sustaining-change-what-s-the-role-of-general-practice