Chronology
2008
Background
Gordon Brown PM
Global financial crisis
Burma cyclone/Chinese Earthquake
Beijing Olympics
Russian/Georgian conflict
NHS events
Alan Johnson SOS
Regional (Darzi) reviews
Final Darzi Review Report, High Quality Care for All
2009
Background
Israeli invasion of Gaza strip
Barack Obama President of USA
Parliamentary/MP financial scandals
UK Population 61 million
Copenhagen climate conference
NHS events
NHS Constitution
Mid-Staffordshire Report on poor-quality health care
Care Quality Commission takes over from Healthcare Commission
Andy Burnham Secretary of State for Health
Financial stringency – Nicholson Challenge to save £20 billion
Swine flu concern and mass immunisation
Prime Minister’s Nursing Commission
2010
Background
Haiti earthquake
Obama’s historic US health care plan
Election – LibDem/Conservative coalition, David Cameron PM
Gulf of Mexico BP Oil spill
iPad launched
NHS events
Andrew Lansley SOS
Equity and Excellence, liberating the NHS
Healthy Lives, Healthy People – public health White Paper
Royal Centre for Defence Medicine (Birmingham) replaces military hospitals
2011
Background
‘Arab Spring’ uprisings in Tunisia, Egypt, Yemen, Syria and Libya
Japanese earthquake/tsunami/nuclear power station problems
Widespread riots in English cities
Euro/Greek financial crisis
NHS events
Health and Social Care Bill
“20 Trusts with major cash problems”
2012
Background
London Olympics
NHS events
Passage of Health and Social Care Act
Jeremy Hunt Secretary of State for Health
2013
Background
Cyprus financial problems
NHS events
New structure introduced in April
111 emergency phone system introduced
2014
Background
Russia annexes the Crimea
Scots vote to remain in the UK
Multiple Middle East conflicts & emergence of ‘Islamic State’
UKIP make progress in polls
Marriage (Same Sex Couples) Act
NHS events
Simon Stevens new Chief Executive of NHS England
NHS England 5-year view
Ebola outbreak in West Africa
2015
Background
Conservative election victory
‘Islamic State’ & European migration crisis
NHS events
Greater Manchester decision to merge health and social care budget
2016
Background
UK votes to leave the EU (Brexit)
USA elects Donald Trump as 45th President
NHS events
DevoManx inaugruated
Sustainability and Transformation Plans (STPs)
2017
Background
General election. Conservative majority eliminated
NHS events
Jeremy Hunt Secretary of State for Health
Move to explore Accountable Care Organisations
The seventh decade
In the seventh decade of the NHS, the costs of healthcare continued to rise, fuelled by an ageing population, greater public expectations, the high cost of new treatments, air pollution and, in the view of many, worsening social determinants of health.
Yet, at a time of rapidly escalating demand, a disruptive, demoralising and distracting reorganisation was imposed during a period of economic crisis. A worldwide financial problem in 2008 had rapidly escalated. A crisis in the USA caused by ‘sub-prime’ mortgage loans, repackaged as ‘derivatives’ on which there was default, escalated into global economic recession. Tax revenues fell and social security payments rose. The housing market was depressed for a while, though in the south properties were increasingly unaffordable while appreciating partly because of an influx of foreign property investors. Labour’s control of the NHS ended in May 2010 when the party polled just a few seats fewer than the Conservatives who, in coalition with the Liberal Democrats, formed the new government. The Coalition imposed economic stringency to reduce the deficit and, five years later, the Conservatives won a surprise majority as the country emerged slowly from recession, Jeremy Hunt remaining Secretary of State. In his first major speech, David Cameron, again Prime Minister, pledged improvement of care outside the hospitals and, for the hospitals themselves, a full seven-day service. His decision to call a referendum on membership of the European Community led to a majority for ‘Brexit,’ triggering his resignation and a new Prime Minister, Theresa May. The United Kingdom Independence Party (UKIP) increased its strength and had attained its main objective.
The life pattern of the technological younger generation differed from that of their parents. If in work, they were insecure; they married later and had fun in the meanwhile. Social media multipled. Family responsibilities were postponed. With the rise of cohabitation, the ‘single never married’ showed the greatest rise of any census category, 35 per cent of the over-16s. The population of the UK was increasing by some 400,000 a year, half because of an excess of births over deaths, half an excess of immigration (some 500,000 a year) over emigration. London was the most popular destination, with an increase of about 100,000 a year, for it provided employment for a myriad of European citizens facing unemployment in their own, often Southern, European countries.
Public sector workers took strike action against the cutbacks imposed by a governments dealing with the recession. Social attitudes were changing; there should be “no more something for nothing”. The United Nations’ eight millennium development goals, for example, combating hunger, child mortality and AIDS, were unlikely to be met as rising food prices and the cost of oil pushed millions more into poverty. In 2011, the Arab Spring culminated in uprisings against autocratic regimes in Tunisia, Egypt, and Libya. The radical ‘Islamic State’ emerged as Syria and Iraq experienced a full-scale and frightful civil war, culminating in mass migration. Russia annexed the Crimea. Natural disasters, such as an earthquake in Haiti with 200,000 dead, and an Ebola crisis, stretched aid agencies.
A historic decision under Obama set in train a continuing process of extending health coverage by the Affordable Care Act to almost all of the legally resident USA population, and created incentives to contain the unaffordable growth of US health care costs. The attempts by his successor, President Trump, to overturn the plan largely failed.
If, in the sixth decade, the NHS seemed dominated by the turmoil of Labour’s multiple reorganisations, the seventh was worse. The five years of the coalition government fell into two halves. The first was devoted to the debate on, and passage of, the Health and Social Care Bill, designed to increase competition and devolve decision-making. The second was a damage-limitation exercise following Andrew Lanlsey’s disastrous reforms, with attempts to handle increasing financial problems, a process continuing under the Conservatives after election. Continuing stringency and the knock-on effect of cuts in local authority social services exacerbated problems.
Public satisfaction with the NHS was, however, stable.1 The National Centre for Social Research had conducted annual surveys since 1983.2 When Labour had entered office in 1997, only a third of people (34 per cent) were satisfied with the NHS. By 2009, satisfaction stood at 64 per cent and was 70 per cent in 2010, the highest level since the survey began. The reduction in waiting times for hospital inpatient and outpatient services was primarily responsible and the increased allocations to the NHS had probably helped. In 2016, public satisfaction with the NHS was 63 per cent, still high by historic standards. Satisfaction was broadly the same as in 2015, and could be split into three phases: ‘steady growth’ from 2002–2010, ‘a sudden drop’ in 2011, and ‘little change’ from 2012–2016.
Health services internationally were hit by a ‘perfect storm’. Money was tight but people’s expectations were increasing in a ‘me too’ society. Technology was providing a growing number of expensive treatments, radiotherapy was far more precise and effective, imaging of a quality unbelievable only a few years previously, and some 40 new drugs for cancer were in the offing, each costing some £2,000–3,000 a month. The population was ageing, bringing increased costs, and death was seen as ‘optional’ – to be postponed if enough money was spent. How could one pay for the triumph of medicine? Increasingly problems in the elderly, which required both health and social care, led to the idea of unifying the system and, in 2015, the Coalition (in a surprise decision) decided to implement this in Greater Manchester using regulations rather than an Act to make it possible.
The 60th anniversary in 2008 was widely commemorated. Health Service Journal listed the 60 people considered most influential, Bevan being the winner.3 Few publications celebrated clinical developments or the improving service to patients, and most dealt with macro issues of politics and funding. Parliament’s The House magazine produced a supplement on the Secretaries of State of the previous 30 years, and articles by each one.4 Frank Dobson attacked the health policies of his party and its accent on the marketplace. Alan Milburn believed that devolution had not proceeded far enough and suggested that the better local authorities might undertake health service purchasing. The King’s Fund produced an analysis of changing workload, finance and waiting times over 60 years. 5 The Nuffield Trust published Rejuvenate or Retire, in which senior figures mused on the past performance and future possibilities and agreed that the NHS should remain taxpayer-funded and free at the point of use.6 When radical alterations had been raised 20 years previously with Mrs Thatcher, Sir Kenneth Stowe, then Permanent Secretary, recalled her saying, “There is no constituency for change”. Most agreed with the purchaser–provider split, that the private sector offered important competitor services within the NHS, and that more decisions should be taken locally. None predicted the financial crash only months later, which had a massive effect on the NHS and all public services.
The four UK Health Ministers restated the principles of the NHS: a comprehensive service available to all; access to services based on clinical needs and not on the ability to pay; aspiration to high standards of excellence and professionalism; NHS services reflecting the needs and preferences of patients, their families and their carers; working across organisational boundaries with other organisations in the interests of patients, communities and the wider population; commitment to the best value for taxpayers’ money; making the most effective and fair use of finite resources; and accountability to the public, communities and patients that the NHS serves.
Labour had followed the Conservative’s Patients’ Charter with a ‘Constitution for the NHS’, pulling together existing rights, responsibilities and pledges, the right to make choices about their care and “to expect local decisions on funding of other drugs and treatments to be made rationally following proper consideration of the evidence”.7 When published in January 2009, the response was lethargic.
Reviewing Labour’s reforms
Throughout the previous decade, Labour had introduced one reform after another. Now it was stocktaking time. There had been four important innovations: Foundation Trusts; greater NHS use of the independent sector; patient choice; and payment by results. RG Bevan wrote that “healthcare systems had three main goals, to control total costs, to achieve equity in access by need and to achieve excellence in performance (short waiting times, satisfied patients, and good outcomes)”.8 The problem was improving the performance of providers. Before 1991, the NHS had a hierarchical integrated model in which the same organisations were responsible for determining the needs of their populations and for running providers. Such organisations could be funded equitably for their populations or for the performance of providers, but not both. The internal market with a purchaser–provider split, in which purchasers were funded for their populations and contracted with independent providers, was an attempt at an answer. England had tried four variations of this model to improve provider performance: competition between 1991 and 1997; partnership between 1997 and 2000; publishing performance in ‘star ratings’ between 2001 and 2005; and again competition from 2006, changing the methods of payment. In June 2008 the Audit Commission published Is the Treatment Working?.9 The development of Foundation Trusts and patient choice was behind schedule, and the scale of independent sector treatment centres was limited.
Scotland, Wales and Northern Ireland had different systems as a result of the devolution of health service management to the four nations of the UK. Marked differences were emerging in hospital services. Policies led to different incentives. In England, targets to improve performance, payment by results and the increasing emphasis on the provider/commissioner split and patient focus had driven change. Scotland had abolished the internal market and had integrated boards, purchasing and providing primary and secondary care; Wales did not separate purchasers and providers either, was looking at the Scottish model but was experiencing major waiting list problems; and Northern Ireland continued with its integration of health and social services. Several studies showed that, compared with the others, England had shorter waits in Accident and Emergency (A&E), even though the reduction of waiting times seemed associated with a greater rise in attendances than elsewhere. Proportionately, more patients were discharged rapidly, within a day of admission, in England.
In 2010, Nuffield reviewed their experiences, suggesting that England was comparatively more efficient, spent less on health care, had fewer doctors, nurses and managers per head of population, and was making better use of the resources it had in terms of higher levels of activity, crude productivity of its staff, and lower waiting times. Three years later, a follow-up report revised this view, suggesting that the different policies adopted by each country appeared to have made little difference to long-term national trends.10 The King’s Fund, in Understanding New Labour’s Market Reforms (2011), felt that Labour had gone much further in introducing changes and encouraging market competition than the Conservatives in the 1990s, the fears then voiced had largely not come to pass, but their impact was also more limited than their proponents had hoped.11 The NHS “was still some distance away from functioning as a fully-fledged provider market for publicly financed care. The system continued to be run by a closely managed hierarchy, while operating in a more market-like way in specific respects.” Hawkes wrote that the reforms had emerged piecemeal for, while there were policy statements, a clearly articulated plan was never put before Parliament or the electorate, in part because it avoided a showdown in the Labour Party ranks, not least between Blair and Brown who differed substantially on issues such as patients’ choice. “The reforms worked but the politics of the reforms was a disaster.”12
Before losing power, Labour still had shots in its locker. In May 2008, Lord Darzi published Leading Local Change:The Next Stage Review.13 His final report, High Quality Care for All, appeared at the time of the 60th anniversary.14 It was followed by separate strategies on primary and community care, workforce issues and informatics. The key effects of the clinical slant of the Darzi proposals were to press the quality agenda and to raise the profile of service configuration in hospital and community services. The King’s Fund summarised this final report.15
|
London Reports |
National Darzi reports |
|
The case for change (2006) |
|
|
Saws and Scalpels to Lasers and Robots – clinical change (2007) |
Our NHS, Our Future (interim report, October 2007) |
|
A Framework for Action (July 2007) |
|
|
A local hospital model for London (November 2008) |
High quality care for all – Final report (June 2008) |
|
The Shape of Things to Come – Stroke & Trauma consultation (February 2009) |
Andy Burnham (2009–2010), the last of Labour’s five secretaries of state, was a cast-back to Frank Dobson and the old Left. Different parts of the Department of Health now did not seem to speak to each other, and policies seemed increasingly chaotic. The use of competition to drive innovation, quality and choice as espoused by Paul Corrigan,16 a special adviser to Alan Milburn and Tony Blair and later a director in the London Strategic Health Authority (SHA), had become unappealing to No 10. Speaking to the King’s Fund in September 2009, Andy Burnham said that the NHS, not the independent sector, was the “preferred provider”.17 Unite, Britain’s biggest union and a major funder of the Labour Party, had petitioned the government to “roll back the privatisation of the NHS” and claimed a major victory. Burnham argued that reform meant working to improve existing services where they were “good enough”. When the 2010 election came, Labour reaped little advantage from its undoubted achievements.
Health policies under the Liberal/Conservative government
The 2010 election produced a Conservative/Liberal Democrat coalition. Andrew Lansley became Secretary of State and, during the previous six years as Shadow Health Secretary, he had given much thought as to how to achieve his vision of a service in which private, not-for-profit and public providers competed against each other, and GPs commissioned services on behalf of their patients. Lansley arrived with a draft White Paper in his pocket: he had written a Conservative paper NHS Autonomy and Accountability Proposals for Legislation in 2007.18
Coalition government being unusual, joint policies had to be agreed. Danny Alexander and Oliver Letwin worked on a programme for government and had to square the Conservatives’ belief in markets as the way to reform the NHS, and the Liberal Democrats’ manifesto commitment to elected health boards and belief in democracy.19 As far as the NHS was concerned, the outcome, (on which Andrew Lansley had not been consulted), was a muddle. Nick Timmins explored the political manoeuvres as the original attempt to build on Labour policies became revolutionary changes.20 Lansley didn’t like it. His reaction was, “let’s find a way round it. Let’s show how it is unworkable and we can deal with it”. He wished to make his changes hard to reverse. Some of Lansley’s 2007 document was cut and pasted into the White Paper, with proposals such as the abolition of SHAs that had been in the Liberal Democrats’ manifesto.
Many were shocked by the scale of changes, which involved a huge Bill, complicated legislation, major administrative upheaval and a pitched battle with professional interests. It was not clear what the ‘reforms’ were designed to achieve, since public satisfaction was at an all-time high. Many seemed unrelated to the problems facing the NHS: demographics, technology, increasing demand and the financial crisis.21 They were complex, involving complicated and obscure legal provisions. Launched at a time of unparalleled financial problems, they were a distraction from the main task and never secured support from the people on whose agreement they depended. So began a two-year process, perhaps the messiest reorganisation the NHS had ever undergone, although the events prior to the 1974 reorganisation came a close second. Following the longest period of sustained spending increases in NHS history, stringency now struck so the NHS had enough to handle without major structural changes. Though the health service budget was ring-fenced, finances would be tight and management costs had to be reduced. Lansley was no believer in strategic planning and wished to reassess the Darzi-inspired London NHS restructuring. The chair of NHS London, whose vision of the future of London’s NHS had been painstakingly worked out and differed from Lansley, resigned in protest as much useful work was halted.
Equity and Excellence: Liberating the NHS
In July 2010, Andrew Lansley published his White Paper Equity and Excellence: Liberating the NHS.22 The major themes built on the internal/social market model. It had taken 50 days to bring forward proposals, compared with ten years for the Conservative administration in 1990 and six years for Labour in 2002. David Nicholson, the Chief Executive of the NHS, said “nothing in the system is left untouched”. 23 There had been no warning in speeches, manifestos or even the Coalition agreement of the scale of the change. They were immediately criticised by some as creating unnecessary turbulence, but early opinion was unconventionally split, with some ex-Labour advisers supporting the proposals and right-wing think tanks opposing them.
The Bill’s stated aims were to strengthen commissioning of NHS services, increase democratic accountability and public voice, liberate provision of NHS services (that is, make it easier for private organisations to provide services), strengthen public health services and reform health and care ‘arm’s-length bodies’. The ‘vision’ was a service delivering good outcomes and devolving decision-making to the front line. The encouragement of “any willing or qualified provider” led to concern that competition and “privatisation” of the health service were in Lansley’s mind and the regulations that ultimately came into force, increasingly opened up the NHS to competition from private providers. The abolition of the SHAs and the Primary Care Trusts (PCTs) removed all the bodies that had a responsibility to plan in a strategic way in accordance with a population’s need. National and regional specialist services would be commissioned by a new NHS Commissioning Board – NHS England – taking over many SHA functions.
On the commissioner side, 500–600 consortia of GPs would take responsibility for most of the NHS budget, transferred from PCTs. No other country had placed such emphasis on GP purchasing. A £20 billion efficiency saving by 2014, a reduction of 45 per cent in management costs, and a reduction in the number of management bodies was promised. Lansley’s 2007 paper had said: “We support the return of powerful, clinician-led commissioning in primary care – like that engendered by GP fundholding in the 1990s.”
On the provider side, NHS Foundation Trusts would have greater autonomy and independent sector providers were encouraged to compete for patients. There would be no cap on the income NHS Trusts could generate from private practice. The operation of the market would be overseen by an economic regulator, a new role for Monitor. Monitor would promote competition, regulate the prices paid to providers and ensure continuity of service provision. Public health functions would move to local authorities who would employ a director of public health and have a ring-fenced public health budget. Local authorities would also be given control over local health improvement budgets, and the power to agree local strategies to bring together the NHS, public health, and social care. Council-based public health teams would provide commissioning consortia with information, evidence, needs assessment, and the quality improvement support needed to commission integrated health services. Local authorities would establish Health and Wellbeing Boards to lead on improving the strategic co-ordination of commissioning. Patients would get more choice and control, so that services were more responsive and designed around patient needs. They would be able to choose their GP practice regardless of where they lived, and choose between consultant-led teams. More comprehensive and transparent information would help them. Management costs would be reduced so that as much resource as possible supported front-line services. The NHS would aim for outcome measures of quality rather than process measures or targets; GPs and hospitals would have to publish detailed outcomes of their care, including medical errors. Those commissioning care had to consider bids from well qualified private providers, and an increasing number of contracts subsequently went to the private sector – sometimes for clinical services, including community health services, out-of-hours GP services and (in the case of Hinchingbrooke), an entire hospital. Many changes did not need legislation. PCTs could and were merged. Separate commissioning and provider functions were established within the Department and within the SHAs to guide implementation.
The King’s Fund believed the extent of change was substantial and the pace rapid. Its Chief Executive, Chris Ham, wrote that the changes took forward reforms set out by Labour in 2002 and developed by Ara Darzi in 2008, and were both ambitious and risky.24 Following consultation, the Bill was published in January 2011. It was long and complex. Labour and health trade unions including the British Medical Association (BMA) and the Royal College of Nursing (RCN) were strident in their criticism as was the Royal College of General Practitioners (RCGP). In April 2011, the all-party Commons Health Select Committee, in a thoughtful review, demanded significant changes to accountability and that commissioning bodies should “reflect the range of other (clinical and non-clinical) considerations, including nurses and hospital doctors”.25 Commissioners must be able to facilitate necessary service reconfigurations. The reforms lacked a “strong narrative about why the inevitable upheaval they involve will be worthwhile”. The arguments often seemed either highly complex and technocratic or vague. In retrospect, senior Tories regarded them as the greatest mistake they had made in government.26 Reducing bureaucracy was a popular idea, but not strong enough, and the argument that the NHS had poor outcomes had often unravelled. The government had not made the case that this particular set of reforms was the answer.
Opposition mounts
 An increasing wave of opposition, the report of the Select Committee and the views of some Liberal Democrats, led Andrew Lansley and David Cameron to “pause, listen and engage”. An NHS Future Forum was appointed under Stephen Field to examine the key issues. The process was becoming messy and many felt that Andrew Lansley, by attempting major reorganisation at the time of financial crisis, was living in a parallel universe described unkindly as “la la land”. The Forum reported in June 2011 with “deep seated concern”, believing that the Secretary of State should remain ultimately responsible for the NHS, commissioning consortia should include hospital doctors and nurses, their board meetings should be public, and stress should be placed on an integrated service.27 It doubted whether the correct place for public health in England was within the Department of Health. In their response, Ministers accepted most of the suggestions.28 The Right suggested that easing back on competition made it harder to achieve efficiency and the Left that the earlier proposals had been ill-conceived. Alan Milburn, the reforming erstwhile Labour Secretary of State, saw the modifications as unfortunate. The Times thought that the creation of clinical senates, health and wellbeing boards and other new machinery represented a victory for bureaucratic process and would slow change, rather than open the way to more efficient care.29 Many amendments were made to the Health and Social Care Bill in the Lords and it was referred back to Parliament for reconsideration. The British Medical Journal (BMJ) outlined the main remaining controversial issues such as privatisation, the role of Monitor and the responsibilities of the Secretary of State.30 The Future Forum remained in existence for another year, considering education and training, public health, information and integration.
An increasing wave of opposition, the report of the Select Committee and the views of some Liberal Democrats, led Andrew Lansley and David Cameron to “pause, listen and engage”. An NHS Future Forum was appointed under Stephen Field to examine the key issues. The process was becoming messy and many felt that Andrew Lansley, by attempting major reorganisation at the time of financial crisis, was living in a parallel universe described unkindly as “la la land”. The Forum reported in June 2011 with “deep seated concern”, believing that the Secretary of State should remain ultimately responsible for the NHS, commissioning consortia should include hospital doctors and nurses, their board meetings should be public, and stress should be placed on an integrated service.27 It doubted whether the correct place for public health in England was within the Department of Health. In their response, Ministers accepted most of the suggestions.28 The Right suggested that easing back on competition made it harder to achieve efficiency and the Left that the earlier proposals had been ill-conceived. Alan Milburn, the reforming erstwhile Labour Secretary of State, saw the modifications as unfortunate. The Times thought that the creation of clinical senates, health and wellbeing boards and other new machinery represented a victory for bureaucratic process and would slow change, rather than open the way to more efficient care.29 Many amendments were made to the Health and Social Care Bill in the Lords and it was referred back to Parliament for reconsideration. The British Medical Journal (BMJ) outlined the main remaining controversial issues such as privatisation, the role of Monitor and the responsibilities of the Secretary of State.30 The Future Forum remained in existence for another year, considering education and training, public health, information and integration.
By January 2012, medical and nursing professional organisations had become implacably opposed to the Bill, mainly because of the increased role that competition would play, but also because of the turmoil engendered when management effort was needed to handle major financial problems and the possibility that some changes could reduce the comprehensive nature of the NHS. Changes in NHS pension schemes were also significant. “The upheaval had been unnecessary, poorly conceived, badly communicated, and a dangerous distraction at a time when the NHS was required to make unprecedented savings” said the BMJ.31 Opposition increased, even within the Cabinet, the Prime Minister threw his authority behind the Bill, organisations such as the BMA, RCN and RCGP found themselves excluded from meetings, the Liberal Democrats sought more and more modifications, but eventually after over 2,000 amendments, the Act was passed in March 2012. Andrew Lansley was known to have commented that he could have achieved most of what he had wanted without legislation.
The Health and Social Care Act
Main legislative changes
- PCTs and SHAs abolished as part of a radical structural reorganisation, with new health and wellbeing boards being established to improve integration between NHS and local authority services.
- Clinical commissioning groups (CCGs) to take over commissioning from PCTs and work with the new NHS Commissioning Board, NHS England, in doing so.
- Monitor to regulate providers of NHS services in the interests of patients and prevent anticompetitive behaviour.
- The voice of patients to be strengthened through the setting up of a new national body, Healthwatch, and local Healthwatch organisations.
- A new body, Public Health England, to lead on public health at the national level, and local authorities to do so at a local level.
- The secretary of state retains ministerial accountability to Parliament for the provision of the health service.
- New duties emphasised the need to promote research within the NHS and strengthen requirements to promote education and training.
Source: Health and Social Care Act32
The continuing development of health policies
Unstable, complex and obscure in its hierarchical relationships, the NHS did its best to make an inherently unworkable system work. The appointment of Jeremy Hunt as Secretary of State for Health in September 2012 marked the beginning of a slow process of restoring practicality to the service without an apparent U-turn. The creation of NHS England in 2013 was intended to distance the NHS from the political landscape. In practice problems landed on the desk of the Secretary of State as they had always done, and the Department intervened.33 New policy concepts emerged from many quarters. Announced in 2013, the Better Care Fund earmarked £3.8 billion to create a single pooled budget between health and local authorities. It was to improve the care of vulnerable individuals aiming to keep them out of hospital. It was expected to save a £1 billion and provide an opportunity for improvement, but assessment by the Public Accounts Committee in 2015 suggested mismanagement and found the savings achieved to be derisory. Early on the scene was Labour whose Shadow Health Secretary, Andy Burnham, announced a Whole Person Care approach, in line with the Michael Marmot health inequalities agenda. The vast majority of NHS funding would be handed to local authorities as an integrated budget for most health and social care − perhaps £90 billion. Health care would return to local authorities and their new Health and Wellbeing Boards. National services and primary care would still be commissioned centrally, but most spending would be under council control. In September 2014, the King’s Fund published its final report on the Future of health and Social Care in England. Chaired by Kate Barker, who came from a background of economics and finance, it drew attention to the apparent injustice of care costs for some conditions being free, and others (such as dementia) being costly to the patient. It suggested a ring-fenced budget unified for health and social care, free social care for those with critical or substantial needs, a variety of tax increases and a flat rate of prescription charges with no exemptions to meet the expense. A new dogma was unification of health and local authority care services, which seemed at odds with the purchaser–provider split.
Repeatedly it was said that the NHS had to change. But change into what? Some argued for the closure of many hospitals and a major transfer of care into the community. In July 2013, David Nicholson then Chief Executive of NHS England announced a major review of strategy over the long term – was the purchaser–provider split really appropriate when organisations such as Kaiser-Permanente did well without it? Did every Trust have to be a Foundation Trust? His review was overtaken by events. Financial stringency was still needed and the ‘Nicholson Challenge’ was rolled forward in The NHS Belongs to the People, which set out the problems, quality, patient experience, dementia and the increasing number of the elderly.34 A funding gap of £30 billion by 2020 was identified. David Nicholson had long had an ambivalent relationship with Andrew Lansley, and resigned as Chief Executive of NHS England. In his exit interview in 2014, he gave a damning account of how current NHS rules and structures were obstructing vital changes. “It’s not clear now who makes the decisions… If you’re going to make a big and ambitious change, who actually does it? That’s a real problem.35 To replace David Nicholson, an international search led to the appointment of Simon Stevens. Stevens was a fascinating appointment for he had been central to Labour’s earlier reforms. He had been plucked from obscurity years before by ‘Old-Labour’s’ Frank Dobson, but it was with Alan Milburn that he flourished. He had been a policy adviser to both Tony Blair and Alan Milburn, and he subsequently had extensive international experience. He had largely written The NHS Plan, introducing Primary Care Groups (PCGs) and later PCTs, then moved to become Tony Blair’s health special adviser.36
Stevens’ views differed from those of his predecessor. Speaking to the Commons Health Committee in April 2014, he said that he was a pragmatist, and saw advantages in competition. He thought that the merger and closure of small hospitals in the already centralised NHS might not always be wise, and that CCGs might take more responsibility for commissioning primary health care. Did all acute hospitals need a full complement of trainee doctors? Many European hospitals had consultant provided health care. Was there a case for multi-specialty groups uniting specialist, primary, community and social care with a population-based budget? As economic growth returned, he expected NHS funding to increase in real terms. In October 2014, NHS England published a Five Year Forward View.37 Even with savings on a massive scale, above-inflation rises in funding would be required. Wanless had pointed 12 years previously to the need for full engagement of people in maintaining their own health. They had not done so. The cost of obesity, smoking and alcohol misuse had to be cut. The NHS and the private sector should assist in health promotion.
The traditional divide between primary care, community services, and hospitals – largely unaltered since the birth of the NHS – is increasingly a barrier to the personalised and coordinated health services patients need. And just as GPs and hospitals tend to be rigidly demarcated, so too are social care and mental health services even though people increasingly need all three. Over the next five years and beyond the NHS will increasingly need to dissolve these traditional boundaries.
Barriers between primary and secondary care could be reduced by specialists working in proximity with GPs in the latter’s facilities (a multi-specialty community provider), or by hospitals taking over GP clinics and A&E departments uniting with out-of-hours services (as a primary and acute care provider). A standard pattern across England, such as the district general hospital (DGH) concept, was outdated, and a ‘one size fits all’ policy was no longer ideal. More investment in primary care was needed.
In 2014 the Secretary of State asked Sir Stuart Rose, from Marks and Spencer, to advise on how to attract and develop talent from inside and outside the health sector into leading positions in the NHS. His report – Better Leadership for Tomorrow – was critical; there was insufficient management and leadership capability to deal effectively with the scale of challenges faced. He also asked Sir David Dalton to look at how to end the isolation of failing hospitals from good management and practice, and how to enable the best-performing NHS organisations and most successful chief executives to establish national groups of hospitals or services as beacons of excellence. His report in 2014 saw the need for fast action to maintain providers, and felt that ambitious organisations with a proven track record should help others. Organisations should be part of a local ‘health economy’ and not remain in isolated independence.38 Jeremy Hunt was attempting to mitigate some of the worst of the problems of the Lansley changes. An additional £2 billion was announced for the service. PCGs were looking more like the erstwhile PCTs. Hunt, in an interview with Health Service Journal (HSJ) on 29 November 2014, said that “the market will never be able to deliver in the top priority area of integrated (care) out of hospital”... “choice was not the main driver of performance improvement, contrary to the emphasis placed on it by various governments and senior NHS leaders since the early 2000s... there are natural monopolies in healthcare, where patient choice is never going to drive change”. Emergency services and integrated care were among these.
His Five Year Forward View (2014) and follow-up documents encouraged the development of different models of the provision of care, the consideration of local “health care economies” that spread wider than individual providers and a “success” regime for those in great difficulty. There would be no single nationwide pattern. A dramatic example was the dissolution of boundaries in 2015 in Greater Manchester. From 2016, as part of a move towards devolved government in England, by the deft use of existing regulations and a delegated authority, Greater Manchester would be given control of their entire £6 billion health budget. The tariff and Monitor would be redundant, and CCGs would become budget administrators. Such a unified system had been a gleam in Labour’s eye. The Coalition, and later the Conservatives, rather than Labour would bring it to fruition at least in Greater Manchester.
Gradually, however, the Lansley dream of local autonomy and competition faded. Increased centralisation of guidance and finance, and the financial imperative of keeping within budgets in a harsh climate, brought it to an end.
Organisational structure in 2013
On 1 April 2013, the massive reorganisation of the NHS took place as a result of the Health and Social Care Act. Progressive revisions had increased the complexity and the number of bureaucratic bodies. New ones and old ones overlapped. SHAs and PCTs had been clustered and then abolished. Sir David Nicholson had moved in advance from the Department to become Chief Executive of NHS England, the Commissioning Board. It provided for the first time a statutory division between Ministers and the Department of Health and the commissioning and provision side of the NHS. The new NHS structure was incredibly complex.
The organisations
NHS England
See Parliamentary briefing March 2016 – The Structure of the NHS in England – a factual document with diagrams and some history.
Also NHS England Guide 2014 – Understanding the New NHS – with good organisational diagrams.
Andrew Lansley had designed the NHS Commissioning Board, NHS England, to distance politicians from the day-to-day management of the service and had legislated to remove them from detailed operational matters by restricting their powers under the Health and Social Care Act 2012. Nigel Edwards said that Lansley “appeared to believe that planning – or strategic commissioning – was not just unnecessary but positively bad and viewed SHAs’ planning as being close to a Bond villain in a dormant volcano stroking a cat – it was the sort of top down intrusion against which he had set his face”.
The Act established NHS England as independent and accountable, limiting the power of the Secretary of State, though the concept that government would draw back was soon shown to be nonsense. When any significant problem arose, such as failure to meet A&E targets, Ministers were quick to take charge, leaving NHS England high and dry. Government published a mandate setting out what the Secretary of State expected NHS England to deliver, initially by 2015.39 Five priorities included: improving standards of care; care of the elderly; dementia; multiple long-term diseases; and preventing deaths from the main killers. There were also a raft of subsidiary priorities. Could this be delivered at a time of retrenchment?
The chair, Professor Malcolm Grant, published its manifesto in The Times in April 2013 as NHS England assumed responsibility for the NHS £80 billion commissioning budget.40 NHS England set NHS funding of subordinate commissioning groups, and what the service was expected to deliver in the short and medium term. It had designed the new clinical commissioning system and tried to reinvent the strategic planning function by getting CCGs to work together, by using its muscle as a major purchaser of specialist care or more radically by pushing Academic Health Science Networks as market-shapers. It had four regional branches for London, the North (North West, North East and Yorkshire and the Humber), the South (South Central, South West and South East Coast) and the Midlands (East and West Midlands and East of England.) It operated under a mandate from the Secretary of State, setting out the objectives and policies for the NHS. A more peripheral tier of local area teams later changed to 12 subregions, with functions around the development of CCGs, emergency planning, quality and safety, and service configuration. There were three in London, a north east, a north west and a south London area team, working in a more integrated way. Nationally, ten area teams would undertake specialised commissioning. Once in power, NHS England began to establish policies that seemed to centralise rather than decentralise decision-making. According to the King’s Fund, the system now included many “largely autonomous bodies over which our new chief executive will not have control.”41 It issued much ‘guidance’. Intended to be a lean body, within a couple of years it had 15,000 employees. Monitor, before its merger with NHS Improvement, accused it of “imperial over reach”, as it flexed its muscles over issues such as the control of capital spending by Foundation Trusts.
In a further modification of central management in 2018, NHS England and NHS Improvement planned to work more closely together, with seven regional branches of each, jointly managed by a single regional director.
Public Health England (from 2013)
To “protect and improve public health and reduce inequalities,” Public Health England was established as a central organisation with four regional branches to lead public health initiatives. While not directly commissioning services, it related to the 152 top-tier local authorities which took over the public health budget (£5.45 billion over two years). It established surveillance systems and advised NHS England on campaigns that should be centralised, for example, on smoking and dementia. It supported local government, the local public health system and Directors of Public Health, providing leadership in responding to emergencies where scale was necessary. There had been arguments about whether it could mount an effective public health challenge to policies, being directly responsible to government. It became apparent that it was neither a campaigning body, nor equipped to evaluate policies for which evidence was weak or non-existent, such as annual health checks.
PCTs (ceasing in 2013)
The 2006 mergers had reduced the number of PCTs in England to 151, mostly coterminous with local authorities. They had been responsible for managing around 80 per cent of the NHS budget. PCTs divested themselves of community nursing services and, in roughly equal numbers, these were merged or amalgamated with acute hospital trusts, mental health trusts or aspirant community Foundation Trusts, although a few services went to private sector bidders, two in Surrey to Virgin Care. PCTs and the comparatively few Care Trusts were wound down and often clustered into groups with a single management team before their abolition in 2013.
Clinical commissioning groups (CCGs) (from 2013)
‘General practitioner-led commissioning’ had been a policy since 1991. GPs had a good idea of patients’ needs, their influence might shift care from hospital to the community, reduce the emergency admission rates, and involving clinicians in management was, in any case, a good thing.42 While PCTs had ultimately been responsible for all residents in a geographical area, CCGs would be responsible only for patients registered at practices within that group.
There were already models, (for example, in Northamptonshire) and, by 2012, 257 ‘pathfinder’ groups with populations of 150,000–250,000 covered 97 per cent of the country. General practitioners agreed the membership and representational structure and there was good involvement of most practices. In many cases, the boundaries that emerged were those of the previous PCT.
NHS England determined when the CCGs could take on commissioning and, by March 2013, 211 CCGs covered the country. From 1 April 2013, they became statutory NHS budget holders in their own right. CCGs tended to appoint managers, rather than doctors, as ‘accountable officers’. Initially they were quite small organisations employing 20–30 people, sometimes using commissioning support units to help, but they grew and often merged. Support units could be, but seldom were, private sector organisations – the profit margin available was too small. In most localities, many GPs had a financial interest in a local provider, for example, the organisation delivering out-of-hours care. The risk of a conflict of interest therefore arose. In general, they established themselves remarkably well and developed good relationships with their local providers, and though GPs viewed them more favourably than the erstwhile PCTs, the influence of general practitioners on commissioning was less than most had imagined. The way in which commissioning was organised – dispersing budgets formerly held by PCTs between CCGs, NHS England and local authorities – meant that there was no longer single population-based budgets for health care. A split between primary care and other services at a local level, and between specialised commissioning and general services, created divisions and significant problems. Simon Stevens was supportive of there being increasing commissioning by CCGs and flexibility including co-commissioning by CCGs that were rather too small for some forms of care. NHS England began to devolve the commissioning of the core general practitioner contracts to CCGs in 2017.
Foundation Trusts
First established in 2005, by 2010 there were 130 Foundation Trusts (FTs) and by 2014, 147. The number increased steadily but many Trusts were not well enough governed or in good enough financial shape to achieve Foundation status. William Moyes, the Executive Chairman of Monitor, felt that the performance of FTs had been impressive. A small élite was now exploring the full limits of their potential, with a handful aspiring to be truly world class. They had probably performed significantly better than other Trusts because they were already better managed.
The Health and Social Care Act had only modest effects on FTs. It changed the title of the board of governors to the council of governors. Their management boards would meet in public. Governors were given a duty to hold non-executives to account for the board’s performance and to represent the interests of FT members and the public. Governors could require one or more directors to attend a meeting to provide information on the directors’ performance of their duties, and annual reports must include information on any occasions where this power had been exercised. FTs would also have a duty to ensure that governors had the skills and knowledge to carry out their role.
Much more significant was the increased central direction of all Trusts and the amalgamation of Monitor into NHS Improvement. The accent on competition lessened, and central planning across all providers became more dominant. The difference between FTs and other Trusts was narrowing.
Non-Foundation Trusts
Weaker Trusts could not meet the financial criteria for Foundation status and 99 did not do so by April 2014, the target date for all Trusts to become FTs. Often these had major Private Finance Initiative (PFI) problems. Many more had internal management issues which might not show in the statistics but, because of poor leadership, might be an accident waiting to happen. Some 50 Trusts hoped to become FTs if they received transitional financial support. In 2011/12 they asked for at least £352 million to help them meet Monitor’s financial requirements. Andrew Lansley said such applicant Trusts would have to demonstrate that their problem was: “exceptional and beyond those faced by other organisations”; “historic and that they have a clear plan to manage their resources in the future”; “that they were delivering high levels of annual productivity savings”; and that “they delivered clinically viable, high quality services”. The biggest demand, for £93.5 million, came from a group of non-FTs – Barts and the London, Whipps Cross and Newham Trusts.
The NHS Trust Development Authority (TDA) later subsumed into NHS Improvement
Established in 2013 as a special health authority, the NHS TDA was responsible for those Trusts unable to achieve foundation status and for helping those who might. It grew rapidly, staffed largely by people who had commissioned services rather than by ex-managers. The TDA believed that, of the remaining non-FTs, many were unlikely to be able to stand alone.
Laggard Trusts were groomed to apply. The process was streamlined and included an early inspection by the Care Quality Commission (CQC); a ‘good’ or ‘outstanding’ report was mandatory and the bar to FT status was perceived to have been raised. A rump of nearly 100 Trusts were unlikely ever to be shepherded to FT status and it became increasingly likely that a significant number would end in “special measures” – a failure regime. The TDA became essentially a performance manager mobilising outside staff to assist Trusts whose performance was deficient. Every failing Trust had a different problem requiring different types of assistance.
Bail-out funding continued to be needed and became a function of the TDA, which received bids from non-FTs for £370 million in 2012/13. A significant proportion of such Trusts had no clear plan for sustainability. David Nicholson, on leaving the post of Chief Executive in 2014, said that the policy that all Trusts should become FTs was not going to work. Alan Milburn who, as Secretary of State for Health had introduced FTs, thought that all Trusts should be authorised within three years, and Monitor and the TDA should be combined and charged with helping them. In 2015 it was announced that the TDA and Monitor would be merged and jointly led as NHS Improvement, chaired by Ed Smith and with Lord (Ara) Darzi as a non-executive director. Within this would be a new Patient Safety Investigation Service, based on the principles of the airline industry, and subsuming existing patient safety systems.
Monitor (subsumed into NHS Improvement in 2015)
Monitor’s traditional role had been to authorise FTs, ensure compliance with their terms of authorisation, and to aid ‘provider development’. Following the passage of legislation, Monitor’s core duty expanded to become a regulator for all NHS-funded providers, not just FTs, regulating prices for NHS services, and preventing anti-competitive behaviour against patients’ interests by absorbing the National Cooperation and Competition Panel (CCP). Monitor would ensure that Trusts remained financially sound and well governed.
Monitor not only licensed and regulated NHS FTs, but also licensed not-for-profit and private organisations providing NHS-funded care. It looked at potential breaches of the principles of co-operation and competition – for example, proposed mergers to ensure that a monopoly situation did not arise. When PCTs were told to give up the management of community health services, it examined the bids, and proposals to merge Trusts were examined to see whether alternatives existed within 30–40 minutes driving time. Reviewing in 2013 a proposed merger of head and neck services in Bristol, Monitor felt that the clinical advantages did not outweigh the loss of patient choice.
Whenever commissioners are considering proposals which would reduce the number of providers they should consider the impact that might have for patients. For some services there will be clear clinical evidence to support limiting the number of providers. In other circumstances there may be advantages to having a number of providers. Where the number of providers is limited the process for choosing the providers should be designed to achieve the highest quality and most efficient services for patients and taxpayers, and should ensure that the incentives for improving quality and efficiency are maintained in the longer term. (para 342)
Similarly the merger of two FTs, (Bournemouth/Christchurch and Poole) was blocked because it would reduce patients’ choice, although the Trusts felt it essential to maintain sustainability. In retrospect, both the Department of Health and Monitor thought the outcome unsatisfactory. Stephen Thornton, Deputy Chairman of Monitor, said the competition arrangements were a “bonanza for lawyers and consultants”.
To simplify FT authorisation, the CQC and Monitor integrated their requirements. The Department of Health had powers to direct Monitor should the need arise, and the CQC could direct Monitor to put a Trust into special administration on the basis of quality of services. Where competition between providers was impracticable, as in the case of community and mental health services, competition might exist to provide the service, rather than to provide a second and competitive one. Monitor would guarantee the provision of essential services if providers failed. In 2016, Monitor was integrated with the TDA to become NHS Improvement.
NHS Improvement
Inaugurated in April 2016, NHS Improvement integrated the main functions of Monitor and the TDA. Chaired by Ed Smith, NHS Improvement rebranded, changed the board and chief executive, re-laid the landscape of health care, remodelled regulation, redesigned care delivery along the lines of new models of care, restructured their supporting mechanisms on a subregional basis, merged two organisations, reappraised their workforce, and cut their budget.
Local authorities
Local authorities once again had a significant role in the provision of health care, for example, they were responsible for screening programmes. Because of the inter-relationship of health and social care, £1 billion was transferred from the NHS to them. There were three key areas where the Department of Health wanted to see transferred funding targeted: the protection and development of preventative services; programmes that brought health, economic and social benefits to communities; and the integration of social care and NHS services. Suspicion that this money was used by some local authorities to plug other holes in their budgets led to the examination of this policy.
Healthwatch
A new statutory body called Healthwatch England, an operationally independent committee of the CQC, would have responsibility for strengthening the voice of patients. Local branches of Healthwatch replaced Local Involvement Networks (LINks) and were funded by local authorities.
Health and Wellbeing Boards (new bodies from 2013)
Health and Wellbeing Boards aimed to improve the co-ordination of commissioning across NHS, social care, and related children’s and public health services. Their core membership was defined, and the Department of Health left it to local authorities to decide how they established the boards. They would be public health oriented, developing their own statistical basis. The boards involved local authorities, CCGs, the local patient-based organisation, Healthwatch, public health, social care and children’s services leaders joining together to assess what health and care services local people need, and agree on how they could best work together. Widely welcomed, their impact and influence was variable and generally limited.
Arms-length bodies
Liberating the NHS, Report of the Arms Length Bodies Review reviewed the functions of many bodies and confirmed the continuing existence of some, for example, Monitor and the CQC.43 Others were scheduled for run-down. The Health Protection Agency and the National Treatment Agency for Substance Abuse became part of Public Health England, an executive agency of the Department of Health.
Health and social care sharing
For several years, think tanks and political parties had seen joint working between health and social care services as essential if people, in particular the aged and those with chronic problems, were to be kept well and independent as long as possible. Small experiments had taken place locally as in Torbay. But in February 2015, a radical Memorandum of Understanding was signed by NHS England, the Greater Manchester Combined Authority and the 12 local CCGs and was supported by NHS providers. (document). It would cover the entire health and social care system in Manchester, a combined £6 billion budget. It included adult, primary and social care, mental health and community services, and public health. Coming into partial effect in April 2015 and full effect in 2016, Simon Stevens said that the landmark Memorandum required no legislation and charted a path to the greatest integration and devolution of funding since 1948. Supported by the Chancellor of the Exchequer, the agreement was welcomed on all sides.
Part of a far wider devolution of planning, from April 2016, power to manage the £6 billion budget to manage the health and social care budget was devolved. FTs surrendered their autonomy. GPs were no longer independent businesses but part of locality focused hubs, and GPs would be leaders in local care organisations running primary, community, social and mental health care services. Manchester would do things differently, but national strategies for health services would still apply. The changes would be evaluated and NHS could take back control if necessary. The mergers of CCGs and the establishment of ten local care organisations responsible for delivering primary and community services, built around populations of 30,000–50,000 people, showed it was practicable to change organisational models. While substantial annual transformation money of £150 million for five years was available, the providers were on course for a deficit of £34 million in 2017/18.
A series of smaller pilots announced in 2015 would permit some local authorities and CCGs to integrate particular services within a common budget.
Sustainability and Transformation Plans (STPs)
In 2014, against the background of falling resources, Trusts increasingly in deficit, and fragmented commissioning responsibilities, NHS England began a quiet reorganisation possible within its remit, without legislation or publicity. The NHS Five Year Forward View was published, emphasising prevention, integration of services and putting people in control of their health, and describing new care models. Most models involved closer and different relationships between providers, NHS Trusts, and local authorities. The two principles now appeared to be collaboration, rather than competition, and a move towards integration of health and social services to aid the care of the elderly and those with disabilities and long-term problems. While the 2012 Act had removed Strategic Health Authorities as regional-level planners, a work-around without legislation was introduced in the form of Sustainability and Transformation Plans (STPs). In December 2015, the NHS Shared Planning Guidance 16/17–20/21 outlined a new approach to “ensure that health and care services are built around the needs of local populations”. STPs were to be produced by the end of 2016, using plans and financial templates, with the triple aim of improving health, improving care and saving money. Forty-four ‘footprints’ were defined, the areas and local leadership often being determined by NHS England and its four regional divisions. The coterminosity that might have been expected in a joint enterprise was not apparent. STP footprints varied in size from 330,000 to over 2 million, and involved many different organisations, each with its culture and priorities. There had been limited public involvement in the process, but there had also been limited involvement of GPs and local authorities in some areas.
STPs had no legal framework or formal accountability and their development was hindered by the lack of a budget, or of free managerial time at the senior levels required. As a driver of strategic planning, STPs were the ‘only game in town’. It was assumed that they would feed into operational planning, though they had been created outside any structural framework. The STP process was reviewed by the King’s Fund in 2016 and their further analysis of 44 of the plans in 2017 fleshed out the nature of the proposals. Most included changing the role of acute and community hospitals to reduce the number of hospital sites and beds, centralise some emergency departments and acute services on fewer sites, and reconfigure the way that specialised services are delivered. STPs describe ambitions to improve care in maternity, mental health, learning disabilities, and children and young people’s services – depending on local needs and priorities. A wide variety of measures to improve productivity and efficiency were included. Many were dependent on capital spending when there was little money to be had. Some proposed shared governance of health and social services. Among the challenges faced were the problems of change in the absence of capital to develop community services or new centralised hospital facilities. There was little evidence that reconfigurations saved money. The ‘footprints’ covered by the STPs were encouraged to appoint a single accountable officer, a difficult position as such officers had neither the authority nor (in most cases) the funds to change matters.
The Department implied that the services covered by an STP might evolve into an Accountable Care Organisation (ACO), a term derived from US attempts to improve health system efficiency. ACOs were characterised by an alliance of providers that collaborate to meet the needs of a defined population. These providers take responsibility for a budget allocated by a commissioner (or alliance of commissioners) to deliver a range of services to that population. They work under a contract that specifies the outcomes and other objectives they are required to achieve within the given budget, often extending over a number of years. The King’s Fund, whose definition this is, published a series of reports – Making Sense of Accountable Care – on pilots as they developed. ACOs might cover social and local authority services, bringing into the system some of the known systemic causes of ill health – housing and education.
Finance and the emerging crisis
Money has often driven change in the NHS. After the Blair ’Breakfast with Frost’ (2000) the growth rate accelerated dramatically. When the economic crisis struck in 2008, the growth rate was cut. This triggered financial crises in the service and the future outlook was bleak.
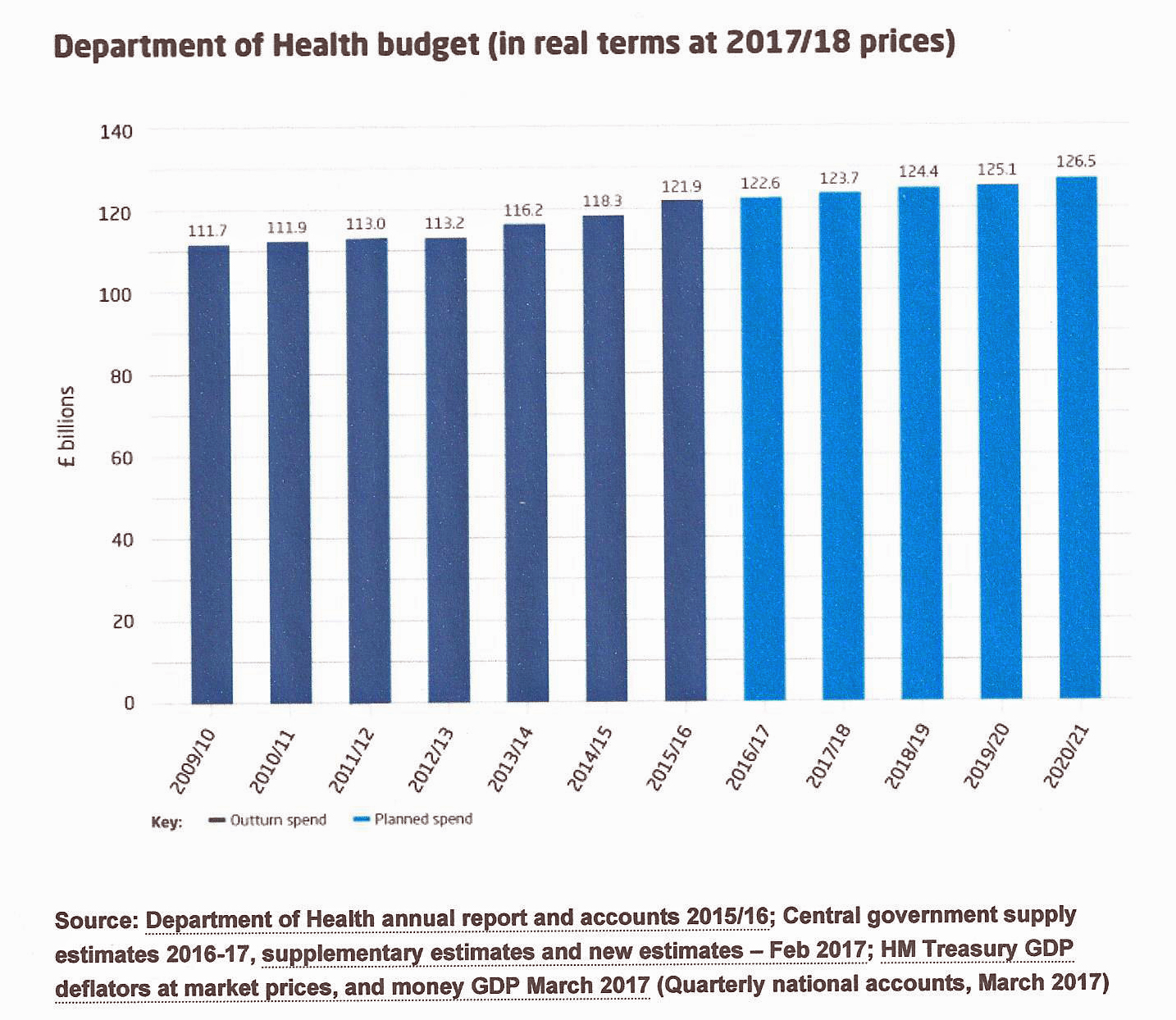
After the previous high growth rate, the projected rise in the NHS budget in real terms from 2008/0 to 2010/11 had been 1.9 per cent a year but, as the financial crisis bit, and billions were poured into banks, projections were reduced to 1.2 per cent between 2011/12 and 2013/14. Public debt would overhang services for ten years or more. David Nicholson wrote:
I first set out the broad challenge the NHS was facing in May 2009 in my publication, The Year: NHS Chief Executive’s Annual Report 2008/09. At that stage we estimated that efficiency improvements of £15–20 billion would be required in the three years between 2011 and 2014. This was based on a broad comparison between the pressures facing the NHS (for example, from pay, prices and growth in underlying demands) and likely levels of funding growth. The range was deliberately a broad one at that point, given the uncertainties, particularly around the level of funding the NHS would receive. Subsequently the Spending Review of 2010 confirmed funding levels for the four-year period of 2011/12 through to 2014/15. Following this we therefore refined the efficiency challenge as up to £20 billion over this four year period.44
The ‘Nicholson challenge’ implied an increase of 4 per cent in productivity annually, and no real-terms increase in NHS budgets. It reflected independent analysis that suggested the NHS would need to sustain large annual productivity increases in order to maintain the quality of its services when health spending was bound to rise more slowly.45 Never had such productivity increases been achieved before. Four chief executives in the London area resigned within a week for financial reasons, including the Royal London and West Middlesex hospitals.
A report for the Department of Health from McKinsey in March 2009 was leaked to Health Services Journal in September and ultimately published by the Conservative/LibDem government in June 2010.46 McKinsey implied that, to achieve its planned £20 billion savings by 2014, the NHS in England would need to slash its workforce by 10 per cent – 137,000. The report revealed the brutal reality of the cost to the NHS of the collapse of the banking system. It recommended a range of “potential actions in the next six months” including a recruitment freeze, an immediate reduction in medical school places to avoid oversupply and an early programme to encourage older GPs and community nurses to make way for “new blood/talent”. Acute services would take the brunt of the cuts. Some savings could come from clinical efficiencies, but not enough. The report (that took the form of a slide series) had the Department of Health’s support and had been shared with SHAs and senior management. McKinsey recommend a nationally-enabled programme delivered through the SHAs and PCTs to drive through efficiency savings. When leaked, the Department attempted to disown the recommendations. Andy Burnham, then the Secretary of State, said “the McKinsey work… is not in any sense an NHS plan of action. They are just making some suggestions which will be looked at with many other ideas.”
Some calculations of the scale of cutbacks – over 50 per cent of London acute hospital work – seemed infeasible. Many hospitals had historic difficulties in balancing their books and this put the quality of care in jeopardy. Over five years, almost a billion pounds was spent keeping some 18 Trusts afloat.
In June 2010, the government appointed an Independent Challenge Group (ICG) of civil service leaders and external experts, to examine the spending review process. In September the group warned that NHS savings might not be achievable and government might face either a growth in waiting times or the need to inject billions more into the NHS.47 Following the Spending Review in October 2010, it was announced that the NHS budget would rise in real terms by 0.1 per cent, keeping the promise to protect the NHS budget, (just).
It was suggested, with little evidence, that massive savings could be achieved by the transfer of care from hospital into the community, polyclinics or federated practices. Small sums were made available for the Transforming Community Services (TCS) programme. Trials showed that telemedicine might make it safe to transfer care of respiratory disease into the community, but there was no evidence of cost saving. Staff of a higher quality might need to be employed in the community setting. The operating framework for 2010 had required a substantial reduction in management costs in PCTs and SHAs, and Acute Trusts would be paid only 30 per cent of tariff costs above the agreed activity level of the previous years. Nor would tariffs be increased for inflation. Health Minister, Mr O’Brien, told Parliament in March 2010 that blaming the economic situation for the cuts was “nonsense”. A manager responded:
Ministers say you must save £20 billion. Ministers then get upset when the NHS puts forward plans to save £20 billion because it involves shutting beds and reducing staff numbers. How else does one save substantial sums of money in a labour-intensive industry? We could of course keep all the beds open and just cut staff – but only if they want a Mid Staffs to pop up every other week.
A pay-freeze for consultants, GPs and senior managers was imposed in 2010, and subsequently for all staff. Financial directors were optimistic that savings targets would be reached in the early years but, when the pay freeze ended, another £500 million would be added to costs. Savings in management costs with restructuring would not be recurrent. Patient care was at risk. Yet the Nicholson challenge was likely to extend for many more years and inevitably this would lead to major reductions in staff. Roy Lilley, in his blog, said that the NHS had been hit with the double whammy of unprecedented and unpredicted demand and the need, like all public services following the credit crunch, to live within its means. The NHS was making its money work at least as hard as the staff on the front line. For 20 years, Jack Wennburg, in the USA, had suggested that reduction in the variations in service provision would save money – though there was little sign of major success in altering the differences, even in his home states. The Dartmouth Health Atlas identified conditions where the rate of surgery differed greatly, for example, osteoarthritis of the knee.48 If there was a £20 billion shortfall in a labour-intensive service, what was the answer? The BMJ published articles on savings that could be made without harming services.49 They did not amount to much.
Evidence of stringency soon appeared. The proposed North Tees Hospital was cancelled. PCTs increasingly controlled the elective admissions for which they would pay, and reviewed procedures, including IVF and reversal of sterilisation and vasectomy and endoscopic procedures of the knee joint, lumbar spine procedures for back pain, removal of breast implants and breast reduction to relieve symptoms.50 When commissioners imposed strict criteria for payment, Trusts might allow patients to purchase care that did not qualify as “self-funded patients”. Such services might include IVF, inguinal hernia and varicose vein removal. The Trusts charged a sum lower than normal private care, perhaps standard NHS prices.
A pay freeze on NHS staff and tariff cuts of 1.5 per cent in 2011/12, a further 1.5 per cent in 2012/13, 1.3 per cent in 2013/14 and 1.5 per cent in 2014/15 was designed to achieve target savings. There was no longer money to reduce waiting lists and they might be allowed to get longer to save money – PCTs sometimes imposed minimum waiting list times. Most Acute Trusts predicted the loss of a substantial number of posts. Whipps Cross in east London, facing a £4.5 million deficit, urged staff to “sacrifice” some of their annual leave or do unpaid work to save money.51 When the reconfiguration of services was seen as a financial salvation, it took time, and the savings did not always materialise. Some hospitals might appropriately close their A&E and move from an acute role to elective work – a regular stratagem to save money – but a temporary embargo on reconfiguration by Andrew Lansley, political pressure from MPs, and public objections made change near impossible.
Between 2009/10 and 2014/15 English NHS funding rose by £14.9 billion from £98.4 billion to £113.3 billion, an increase of around 0.8 per cent in real terms on average, an additional £890 million per year. Yet a looming ‘black hole’ of perhaps £30 billion by 2020 was emerging; Both Trusts and FTswere increasingly in deficit. In the first quarter of 2014, 86 out of 147 FTs reported one and in December 2014 an additional £2 billion annually was found for the service. The Trusts that did not have FT status also reported a combined deficit. Approaching the 2015 election, both parties promised that there would be more money for the NHS; neither could say whether it would be “adequate”. In 2014/15 providers had an aggregate deficiency of over £800 million and predicted worse to come. The King’s Fund reported on the performance of the service under the coalition, finding that it had held up well for the first three years, but had now deteriorated with waiting times higher, and several key targets missed. Public satisfaction, however, remained high.
By 2015 the number of Trusts predicting annual deficits rose – almost half were in deficit. In an autumn spending review, the government made an additional £4 billion available but the National Audit Office (NAO) believed that Trusts as a whole being in deficit, additional money should be used to restore solvency, not to embark upon new initiatives (for example, the 7-day hospital). By early 2016, the proportion of Trusts probably in deficit, some four out of five, and the total deficit likely, led to warnings that, even after Mid-Staffs, head counts could not be regarded as inviolable, and remaining within budget was not ‘optional’. We had moved from a post-Francis accent on quality to recognising that a balance had to be struck between finance and quality. NHS Improvement, the successor to Monitor and the Trust Development Authority, said that “quality and financial objectives cannot trump one another” and that the task of providers was to “deliver the right quality outcomes within the resources available”. In 2015/16 the aggregate deficiency was £2.45 billion and 85 per cent of Trusts were in deficit. In November 2016 the NAO repeated its view (Financial Sustainability of the NHS) of the severe problems faced, and that the short-term measures employed were not a sustainable answer. The pay freeze on NHS staff started to be relaxed in 2018. As the 70th anniversary of the NHS approached in 2018, the government promised an increased growth rate for the NHS over the coming five years, something a little below 4 per cent.
The allocation system
Each year the Department of Health traditionally stated the resources for the NHS and national priorities in its Operating Framework.52 From 2010, this was supplemented by the Outcomes Framework, part of government’s intention to move the NHS away from focusing on process targets to measuring health outcomes. Subsequently a ‘funding envelope’ was agreed between NHS England and the Department of Health alongside the mandate that outlined what the expectations were. For 2013/14 this was £95.62 billion.53 NHS England had to determine how to allocate funds between the main areas of commissioning spend (public health, primary care, CCGs, specialised/health and justice/armed forces and the integration-transformation fund), how to allocate funds within each stream, that is, the distribution between localities, and the pace of change associated with any change in allocation policy. A parliamentary note gave figures for allocations since 1974.54
Area allocations had been based on a complex formula involving population, needs, targets and the distance from targets.55 An Advisory Committee on Resource Allocation (ACRA) kept the formula under review to ensure equal opportunity of access to health care for people at equal risk and to try to reduce health inequalities. As better population data became available, these were incorporated. The National Audit Office produced a report on the system for the Health Select Committee in December 2010.56 The establishment of CCGs in 2013 made it necessary to use GP registered populations, rather than the previous PCT ones, and NHS England began a review of the NHS allocations process, for the formula devised appeared ‘inconsistent’ with the goal of reducing health inequalities. The new and complex system of commissioning which a CCG’s funds depended on included several different income streams, which meant there was a need to balance the total resources available. How was each of these resource ‘pots’ to be distributed geographically, between individual CCGs or area teams, and how did these different strands interact? Resource Allocation Working Party (RAWP) in 1976 had been simple, but the addition of other factors, chronic disease, deprivation and health promotion made for complexity. How should factors be weighted? A ‘fair shares’ formula devised by ACRA considered that the division should relate more closely to age and less to deprivation, creating factions between areas with great deprivation and those with many elderly.
As internationally, most expenditure was spent in the hospitals, and to their inpatient and outpatient services. Day case activities accounted for two-thirds of the NHS spend on hospitals. The highest spending area is emergency care – a total of nearly £14 billion for emergency treatment and non-elective admissions.57 General practitioners said that primary care was responsible for 90 per cent of NHS contacts getting only 10 per cent of the expenditure.
Commissioning
The purchaser–provider split had begun with the Conservatives’ market reforms in 1991, although elements had long existed. An excellent account appears in a House of Commons briefing paper on NHS Commissioning Before April 2013.58 Whereas previously providers, usually hospital doctors, had largely determined what services would be provided, from then on commissioning bodies acted on behalf of patients to purchase the services which were ‘really needed.’ Purchasers were given budgets to buy health care from providers (acute hospitals, and organisations providing care for people.) This split between purchaser and provider underwent changes over the next 20 years, but essentially remained the same. There was an increase in transaction costs, notably management and administration costs. Research commissioned by the Department of Health, but not published, estimated these to be as high as 14 per cent of total NHS costs.59 Commissioning was undertaken at different levels, dependent on the rarity of the condition. Specialised commissioning had long been required at national level and, in 2007, a National Specialised Commissioning Group (NSCG), a National Commissioning Group (NCG) and ten Specialised Commissioning Groups (SCGs) were formed. The complex arrangements were simplified in 2010 when NHS Specialised Services was supported by the Advisory Group for National Specialised Services (AGNSS) but had to be revised again with the establishment of NHS England in 2013.
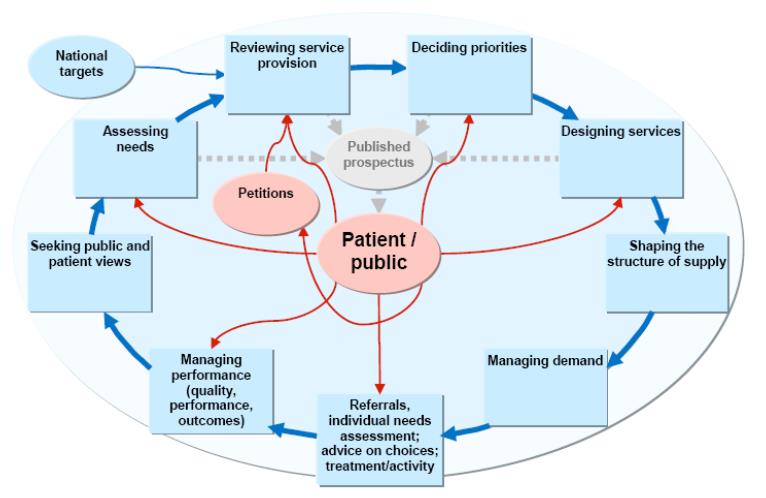
Both Labour and the Coalition had looked at the tariff system for savings. Tariffs had been based on average national costs; should they be based instead on the lower costs of the most cost-effective centres? PCTs were allowed to link payments to local quality improvement goals by commissioning for “quality and innovation”. A proportion of providers’ income would be conditional on quality and innovation, through the Commissioning for Quality and Innovation (CQUIN) payment framework.
The reforms introduced in April 2013 increased the complexity of the commissioning system. Providers found themselves dealing with many agencies:
- CCGss – planned hospital care, urgent and emergency care, rehabilitation care, community health services, mental health and learning disability services
- NHS England – highly specialised services on a regional basis, general medical, dental and pharmaceutical services
- Local authorities – health improvement services, physical activity, sexual health, children, alcohol, tobacco, obesity
- Public Health England advised on health promotion programmes but did not commission them.
Saving money – mergers and acquisitions
Hospital mergers to improve efficiency and save money were nothing new – as far back as the nineteenth century they had been encouraged by the Prince of Wales’ Fund (King’s Fund). Done well, they were a valuable tool to drive better clinical and financial outcomes. But, unlike the commercial field, health mergers were often politically mandated rather than organically initiated, and decisions that should have been taken before merger were approached during implementation. In the commercial field, there was always a reason, for example, the acquisition of assets, an order book or brand names, or the clear possibility of profit. In the NHS, a business case might be prepared, but financial, organisational and political factors might hold sway. Sometimes a merger was seen rather naively as a way out of financial disaster. Other Trusts and FTs were generally wary of the risks involved in taking on the management of a Trust with a financial ‘black hole’. The level of debt made it important to consider staffing levels, as saving money on nurses often led to poor patient care. What Trust wished to jeopardise its reputation by taking on near insuperable financial problems? Easier was the absorption of community services from PCTs, creating ‘vertical integration’ of services. The first Trust opting for merger or acquisition was the Bedfordshire and Luton Mental Health and Social Care Partnership Trust in May 2009, and it became part of the South Essex Partnership University NHS Foundation Trust.
KPMG, in a global study, concluded that due diligence was often skimped in mergers enforced from the top, which were less likely to succeed than those resulting from a local proposal. Timescales were often far longer than had been thought, differences in organisational culture were critical, and mergers between weak organisations rarely worked.60 Historical debt might have to be restructured and successful FTs should be incentivised to acquire others. Obtaining savings often took three to five years.
A study by Bristol University showed that mergers were unlikely to be the most effective way of dealing with poorly performing NHS hospitals.61 The wave of hospital consolidation in the late 1990s and early 2000s, at which time around half the acute hospitals in England were involved in a merger, brought few benefits. Poor financial performance typically continued, with hospitals that merged recording larger deficits post-merger than before. The length of time people had to wait for elective treatment rose after the mergers. There was also no increase in activity per staff member employed in merged hospitals, and few indications of improvements in clinical quality.
Sometimes a merger was considered by Trusts that had not obtained Foundation status and had severe financial and managerial problems. Monitor and its competition panel was wary of some proposals, but others were agreed. Mergers might create hospital giants, for example, Bart’s Health Trust with a £1.1 billion turnover (Barts, Royal London, Whipps Cross and Newham Hospitals).
In December 2011, the Commons Public Accounts Committee questioned whether such reconfigurations would solve the difficulties of the worst performing Trusts and predicted “some form of further intervention” would be needed.62 The committee said it was “already clear that it would be extremely difficult” for the then remaining 113 non-FTs to become FTs by the target date of April 2014. London was singled out for special concern. “We remain to be convinced that combining struggling hospitals into larger trusts – as with South London – will somehow produce viable organisations offering good quality, accessible healthcare”. This view was shared by Simon Stevens on taking over from David Nicholson as Chief Executive, NHS England. England already had a more centralised hospital service than many countries, there was a role for small and medium-sized hospitals, and while for some services such as stroke, the case for centralisation was clear, this approach was not always necessary.
The Trusts with the greatest financial problems were often those most at risk of poor clinical performance.63 There was general recognition that those with large PFI debts might never repay them and, in October 2011, the Department identified 20 whose clinical and financial stability was at risk because of cash-flow shortages and legacy debt. They would “need help to become sustainable for the long term”. One Trust, Hinchingbrooke, a district general hospital in Cambridgeshire with a £40 million deficit, was offered by tender. No NHS organisation would take on the risk. In November 2011, Circle Health did and made substantial progress in reducing its overspending and improving its management. However, in 2015 reduction in tariff payments and rising hospital activity meant that Circle could no longer afford the losses it was picking up. It ended its contract and applied for a £10 million bailout. Bart’s Health Trust sought £22 million annually to manage their PFI debt. By July 2013 it was losing £2 million a week and it notified the TDA. The deficit continued to rise and, in 2015, following a report by the CQC on Whipps Cross, the Chair, Chief Executive and Chief Nurse resigned and the Trust was placed into “Special Measures”.
McKinsey’s assessed which Trusts would need support to enable them to reach FT status; NHS London believed that only a third (six) of its acute non-FTs was financially viable, even after major efficiency programmes. In February 2012, the Department of Health said the cost of bailing out seven Trusts with PFI problems was £1.6 billion – St Helens and Knowsley, North Cumbria, Dartford & Gravesham, South London Healthcare Trust, Barking, Havering & Redbridge and Maidstone & Tunbridge Wells. Peterborough and Stamford FT, though warned by Monitor in 2007 that a PFI scheme was dangerous, nevertheless signed and subsequently required a bailout. In the financial year 2011/12, 31 Trusts needed bailouts of £414 million, some because they could not cope with PFI payments, and others to restore a historic problem before an application for FT status. Similar bailout payments were needed in the two successive years. The 13th Report of the Parliamentary Health Committee in January 2012 said that fundamental change was necessary to save the £20 billion envisaged.64 Four underlying causes of deficits were: inefficiency and poor management; high legacy costs, such as PFI; inappropriate design of payment by results tariffs; and stranded capacity costs that arise when work is lower than planned because of unanticipated shifts in demand and income across Trusts.
‘Failure’ and ‘Success’ regimes
From April 2013, under the Health and Social Care Act, a special administration regime was available for failing Trusts whether FT or not. Failure would be avoided where possible by assessing the risk Trusts faced; identifying Trusts where there was concern; and ultimately provider failure where administration might be necessary. At each stage Monitor would work with the Trust and, in the case of non-FTs, the NHS TDA. Where special administration was necessary, the priority would be to maintain quality services and to plot a way ahead. A central financial risk pool was established to fund administration, services not covered by income, and any restructuring. The Secretary of State could make an order appointing a Trust Special Administrator (TSA) to be laid before Parliament. Normal governance arrangements would be suspended and executives would report to the TSA. Within 45 working days, the administrator had to produce a report for the Minister to lay before Parliament. After a month’s consultation, the final report was presented to the Minister and Parliament and, within a further 20 days, the Minister must make a decision and publish it.
South East London, was first to experience this. Two whole hospital PFI sites (Bromley and Queen Elizabeth Hospital) had long-standing and insuperable financial problems. In 2009, after a five-year exercise (A Picture of Health), a scheme was approved to close emergency admissions with a large reduction in bed capacity at the Queen Mary’s Sidcup site. This affected 284 acute beds with a reduction in medical, nursing and non-clinical staff. Cost-saving was not so easy. In 2012, the recently appointed chief executive who had inherited an impossible problem stood down; the South London Healthcare Trust was looking at a £65 million deficit on a £440 million turnover. It had amassed debts of £150 million and was put into administration by the Secretary of State in 2012. It was the first Trust to go into administration, the administrator being Matthew Kershaw, previously the Department’s director of provider delivery. He reported that the Trust might need to be broken up, its services passed to other neighbouring Trusts, and it could not survive in its current form. He suggested the Princess Royal site in Bromley be merged with King’s College Hospital, closing the emergency department at Lewisham Hospital which had no problems and had not been part of the failing Trust, and merging it with Queen Elizabeth Hospital. Bexley would be passed to Oxleas Foundation Trust. South London Healthcare Trust would be dissolved. There was immediate public protest. “Taking resources from a really good hospital (Lewisham) to prop up hospitals that are not performing well does not seem a logical solution.”The Secretary of State’s agreement to the report was challenged successfully by a local action group and the Department introduced legislation to ensure that TSAs were given wider powers. The lessons to be learned were examined by the King’s Fund.65
This Trust was only the first of a number of Trusts to get into difficulties. A £300 million fund would meet the costs of other Trusts likely to fail. A framework and a system was established, with forensic accountants and staff to handle the problems likely to emerge. As the problems grew a new ‘success’ process was added to the ‘failure’ regime that was having only limited effects. In 2015, Cumbria, Essex and Devon which had long-standing problems were placed in the framework, and a director was appointed to look across the ‘health care economies’ of large areas with many Trusts to draft in experienced support and produce an area-wide strategic plan covering all health and care services.
Quality
The introduction of medical audit in the Conservatives’ NHS reforms, and the establishment of Commission for Health Improvement (CHI) a decade later, began the process of making quality an essential component in the delivery of health services. Quality was being taken seriously by managers as well as clinicians. Progress was halting and, as in the case of the disputes between CHI and the Department of Health, the accent on regulation might conflict with the principles of continuous quality improvement. For the first time, managers might lose their post if their Trust’s care was poor, as quality became as significant as meeting the budget in annual assessments. Lord Darzi, though not personally responsible for this, epitomised the change. He said in 2008 in High Care Quality for All, that “Quality will be the organizing principle of the NHS.”66 The final Darzi report later in 2008 also emphasised quality as “at the heart of everything we do”. Healthcare providers now had to publish ‘Quality Accounts’ just like financial accounts. Quality accounts were submitted initially to the Healthcare Commission and later to the CQC. Their structure was dictated centrally. In general, they were self-completed and were more concerned with structural and procedural aspects of care, and whether the hospital operated appropriate protocols, than the matters of most interest to patients. Analysing a sample of the reports for 2009/10, the King’s Fund said they were extremely varied in choice of measures, the presentation, variation in coding quality, participation in national clinical audits and confidential enquiries, and the extent of local involvement. It was not possible to assess or compare the quality of care of providers from the reports.67 Their aims and the intended audience were vague – the Fund thought the audience ought to be the general public. A fundamental tension at the heart of quality accounts was between requiring content that enabled comparability between Trusts, and allowing providers local flexibility in the information chosen. Each year the system was modified, and it increasingly took into account views of patients and patient organisations, and in the case of FTs, the governors. In addition, there were inspections conducted initially by generalist teams that had little experience of the hospital environment, but after the Francis Report in 2013 (Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry), in greater depth by more expert assessors.
The many facets of quality had always made its assessment difficult. For over 20 years, organisations had wrestled with the problem of how to contract for ‘quality’. The introduction of tariff payments was partly based on the view that if all providers charged the same, those ‘purchasing’ services would do so on the basis of quality, but in the UK, unlike the situation in the USA, there was seldom a wide choice of providers. On the principle that if you cannot measure something, its existence is questionable, a new industry developed in ‘metrics’ – what was quality, how did one recognise it, and how was it measured? Structure, process and outcome had long been recognised as facets of quality; now effectiveness, safety and patient experience were seen as topics for assessment. Patient reported health outcomes (PROMs) were first published in September 2010 by the NHS Information Centre, and from April 2013 by the Health and Social Care Information Centre. These showed that those undergoing joint surgery experienced improvement in 80–90 per cent of occasions, (varicose vein and hernia surgery patients showing less benefit).
Patient participation
A new system to encourage patient participation in assessing the quality of services, LINks, was introduced in 2008. Each LINk related to a matching local authority, the LINk covering both health and social services with open membership. Each was a network of local individuals, groups and organisations covering all aspects of publicly funded health and social care. Built on existing networks and community activities, they were modestly funded and supported by a ‘host’ organisation (appointed by the local authority.) LINks had the right to be consulted about services and, in many instances, to enter premises and inspect services. Where they had concerns, they could ask organisations to respond to their anxieties. The establishment of these new organisations was halting – LINks varied widely in their attitudes, some believing in co-operative working with local Trusts, others being intrusive and run by people with long-standing grievances, special interests, or political views, often critical of the NHS in general and their local services in particular, LINks proved as transient as their forerunners, and were replaced in 2013 by new local organisations, Healthwatch. The CQC hosted the central component of Healthwatch.
Over 60 organisations in the UK had some claim to undertake inspection or regulation. In 2008, a National Quality Board was established for the NHS. A body of the great and the good, it brought together the Department of Health, the CQC, Monitor, National Institute for Clinical Excellence (NICE) and expert and lay members from Royal Colleges and consumer organisations, so the many regulators came together in one room. Its aim was to bring together senior people interested in improving quality, to align and agree the NHS quality goals, whilst respecting the independent status of participating organisations. It operated at a theoretical level, trying to determine what was happening and the quality of the data available. Simultaneously, a Healthcare Quality Improvement Partnership (HQIP) was formed, to promote quality in health care and increase the impact that clinical audit had on health care quality. It was led by a consortium of the Academy of Medical Royal Colleges, the RCN and National Voices (formerly the Long-term Conditions Alliance).
Confidential enquiries
As part of the review of arm’s-length bodies, the four confidential enquiries were examined and their structure, approach and management reviewed. From September 2011, the HQIP became responsible for their management and commissioning, previously the responsibility of the National Patient Safety Agency (NPSA).
Checklists in clinical care
The USA remained a leader in quality developments. Its Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations, established in 1951) introduced patient reports on the safety of care and examined patient care pathways, alongside its 50-year-old accreditation programme. The expansion of clinical knowledge made it essential not only to work in teams, but to accept that medicine’s complexity had overwhelmed the ability of individuals, however expert and specialised. Basic steps were missed and patients died. In aviation, simple pre-flight checklists had saved many planes. The introduction of a surgical checklist in eight hospitals worldwide showed a reduction of death rate from 1.5 per cent before the checklist was introduced to 0.8 per cent afterwards. Nineteen checks before anaesthesia, before skin incision and before the patient left theatre showed that gaps in teamwork and safety practices were substantial in countries both rich and poor. US expertise was recognised when, in 2015, a US$13 million contract was placed with the Virginia Mason Institute in Seattle to improve patient safety and control costs using a lean management system inspired by Toyota, at five Acute Hospital Trusts, including Leeds Teaching Hospitals and Barking and Havering.
Mid Staffordshire
Don Berwick said, “you need policemen even in heaven”. For all the systems of regulation, frightful examples of poor care continued to emerge. That existing mechanisms could not be relied upon was demonstrated at Mid Staffordshire Foundation Trust. In March 2009, the Health Care Commission, following a series of patient complaints and allegations of high hospital mortality, published a swingeing report into substandard care at the Trust. The Trust had a large financial deficit and new management had corrected this in part by staff reductions, including nursing. The financial problems were solved, but at the cost of a failure to address quality which had been a long-standing issue. Mortality data from Dr Foster had suggested problems that were subsequently confirmed. There was a tangled tale of coding changes, challenges to the validity of Hospital standardised mortality ratios (HSMRs), and false reassurances, leading to delay in tackling fatal failures of care. That Foundation status had been granted in 2008 when problems were already being investigated made clear the lack of communication between Monitor, the SHA and the Healthcare Commission. The regulatory organisations blamed each other. Theoretically, because of excess mortality at the hospitals, as many as 400 people might have died over a period of years. There had been “appalling” emergency care in understaffed departments, inadequately skilled, with deficiencies in ward staffing, equipment and management. Professor Sir George Alberti, national clinical director for urgent and emergency care, reviewed the Trust’s A&E services and, in July 2009, the Secretary of State (Andy Burnham) asked Robert Francis QC to investigate cases relating to the care that ... causes concern and to the extent that it considers appropriate; to consider whether any additional lessons are to be learned … to consider what additional action is necessary for the new hospital management.
Robert Francis’ report in February 2010 said the board showed a lack of urgency and relied on data systems rather than patient experience.68 The board tended to restrict itself to strategic issues and had too little contact with operational matters. The overwhelming problems seemed to be the provision of basic nursing care. “The experience of listening to so many accounts of bad care, denials of dignity and unnecessary suffering made an impact of an entirely different order to that made by reading written accounts.” Targets seemed to come before quality, and compassionate care was often lacking. There was reluctance by staff at all levels to persist in raising concerns. The report contained three key recommendations, accepted by the government:
- To ask Monitor to exercise its power of de-authorisation over the Mid Staffordshire Foundation Trust.
- To review the arrangements for the training and accountability of executive and non-executive directors of all Trusts, to create and enforce uniform professional standards.
- An independent working group to be set up by the Department of Health to look at the use of comparative mortality statistics in assessing hospital performance.
A further public inquiry was established in 2010 to look at what went wrong in the wider NHS, the regulators and strategic authority that allowed the situation to develop. The report, published in February 2013, (Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry) was comprehensive, making almost 300 recommendations and the summary alone was over 100 pages in length.69 Some, such as a proposal to merge Monitor and the CQC, were not accepted; most were. The report was critical of the culture of some parts of the NHS, with an accent on finance, targets, and unwillingness to hear complaints from patients. While Francis said that “the public are entitled to expect leaders to be held to account effectively when they have not applied the core values of the Constitution,” and the report criticised the work of the SHAs which oversaw Mid Staffordshire Foundation Trust, it included little direct criticism of specific leaders and seemed to many to fudge the extent to which supervisory organisations had proved impotent. It was said that the draft report had been edited to remove unhelpful criticisms.
There were repeated calls for David Nicholson to resign. Monitor put Mid Staffs into administration as it was neither clinically nor financially sustainable. In 2014, the Secretary of State dissolved the FT and, while services would continue to be provided by the hospital, it would be managed by other Trusts.
The Francis report began a wide debate. Perhaps pressure on all Trusts to achieve Foundation status should be slowed, to ensure that the quality being delivered was adequate? The Secretary of State queried some of the key recommendations and the Prime Minister asked Don Berwick, who had been interested in the NHS for over 20 years, to lead a review of all recommendations, the state of patient safety and quality in the NHS, and of how to improve it with the aim of making the NHS a place of zero harm. In the Department’s initial response in March 2013, Patients First and Foremost,70 it was said that the CQC would appoint a Chief Inspector of Hospitals to identify problems and ensure that action was taken more effectively than before, and rate all hospitals as ‘outstanding’, ‘good’, ‘requiring improvement’ or ‘poor’. Unlike the earlier star system, core services would be examined separately, looking at individual components. There would be a statutory duty of candour making it “a criminal offence for providers to provide false and misleading information about performance,” requiring staff to be open with patients and relatives if they believed treatment or care had caused death or serious injury.
Starting with pilots, it was proposed that every student who sought NHS funding for nursing degrees should first serve up to a year as a health care assistant (HCA), to promote front-line caring experience and values, as well as academic strength. HCAs would not face statutory regulation, as Francis had recommended, but they would be subject to national minimum training and a code of conduct. Mike Richards, the first Chief Inspector of Hospitals, believed that, with better data and a better process, inspection could be made to work and the first round would be complete within a little over two years.
Sir Bruce Keogh, NHS England’s Medical Director, was asked to conduct a series of ‘deep-dive’ reviews into other hospitals with mortality rates which had been consistently high for two years or more. These reviews were rigorous and uncovered previously undisclosed problems.71 Following his report, 11 Trusts were placed into ‘special measures’ because of the significance of the problems – North Cumbria Trust, Northern Lincolnshire and Goole Trust, Tameside Foundation Trust, United Lincolnshire Trust, Basildon and Thurrock Foundation Trust, Burton Hospitals Foundation Trust, East Lancashire Hospitals Trust, George Eliot Hospital NHS Trust, Sherwood Forest Foundation Trust, Buckinghamshire Healthcare NHS Trust, and Medway Foundation Trust. Doctors in some of these Trusts seemed demotivated and isolated, both geographically and clinically. Others subsequently joined them – Bart’s Health and Addenbrooke’s as well. Sir Bruce drew a distinction between hospital statistics that suggested a higher-than-average death rate, and identifying patients whose death was avoidable. It was clinically meaningless and academically reckless to use such statistical measures to quantify actual numbers of avoidable deaths. When Professor Berwick reported, he wrote concisely in a few pages and with only ten recommendations.72 He queried the desire to play a ‘blame game.’ He praised the NHS commitment to health care as a human right and said that drama, accusation and overstatement were best avoided. It made no sense to punish someone who made an error; the organisation should learn from it. Government also commissioned a report on the handling of patient complaints in the NHS by Ann Clwyd MP and Professor Tricia Hart that suggested improvements to the system.73
In government’s final response to the Francis report in November 2013, bringing together the recommendations of Bruce Keogh, Ann Clwyd, Camilla Cavendish (on health care assistants) and Don Berwick, it set out a series of measures aimed to ensure that patients knew what the system knew, “whether hospitals are safe, how well they are led and what patients say about their experiences there”.74 In 2014, the Care Act included a statutory duty of candour that required providers to be open and transparent when things had gone wrong. But things continued to go wrong and, in 2017, breast surgeon Ian Paterson was convicted of 17 counts of wounding with intent to cause grievous bodily harm, subjecting patients to surgery that, prosecutors said, no reasonable surgeon would have considered justified. His Trust paid out nearly £18 million in damages and costs to settle 256 claims involving his NHS work.
A different form of problem arose in the wake of the allegations in an ITV documentary exposing Jimmy Savile as a prolific paedophile. More than 100 people came forward giving accounts of their abuse on NHS premises and elsewhere, across 28 hospitals between 1960 and 2010. A report from Leeds in 2014 covered Savile’s 50-year association with the General Hospital where he acted as a volunteer porter, the abuse of at least 60 people and three accusations of rape. Senior staff were repeatedly told, yet no action was taken.
Worst, perhaps, was the report of an Independent Panel on Gosport Memorial Hospital in 2018, which revealed that 450–600 patients had had their lives shortened by a regime of opioid overdosage, many of whom had no life-threatening illness. A series of previous enquiries by the Hampshire police and the health service had failed to reveal the true horrors.
Regulatory bodies
There was an underlying naive belief that regulation could guarantee quality. In short order, three quality regulators replaced each other, CHI, Commission for Healthcare Audit and Inspection (CHAI – the Healthcare Commission) and CQC. Each fell short of expectations, but the obvious conclusion that regulation alone could not be relied upon to guarantee quality seemed unclear to those concerned. Failures of regulation only led to the modification and establishment of new regulatory bodies. There was scepticism of the process for many organisations, Monitor, the CQC and the TDA, all imposed discipline on managers that resulted in pressure on staff to conceal and work around difficulties that could seldom be solved within existing budgets and staff numbers. Assurance that ‘all was well’ now became a priority. Commissioners and providers could not afford to risk becoming the next Mid Staffordshire. Management of risk mattered, but health care is intrinsically a risky business and there could be no guarantees that outcomes would always be perfect. Regular hospital ‘hygiene’ inspections included patient representatives and became more rigorous – for example, Patient-Led Assessments of the Care Environment (PLACE inspections.
The Healthcare Commission (CHAI) 2004–2009
In October 2008, the Commission published its third and last health check assessment. Annual improvement seemed apparent, with more Trusts scoring ‘excellent’ for quality and for use of resources. Waiting times for cancer treatment had come down. Ambulances were responding faster. Methicillin-resistant Staphylococcus aureus (MRSA) rates were falling. Problems remained in primary care, such as access to GPs and the provision of choice. Regionally, performance in most areas had improved, less so in London. Sir Ian Kennedy, in a letter to staff, regretted that relationships between the Commission and the Department of Health had been fraught. “Given the highly politicised nature of any discussion of the NHS, government both saw the need for the regulator and at the same time felt uncomfortable about it, particularly when it brought bad news.” Sir Ian said. “Regulation was sometimes seen as part of the problem rather than part of the solution”. The Commission produced a legacy report.75 It believed that it had played an important part in the improvement of quality of care. Investigations into serious failings had improved safety. The handover from the Healthcare Commission to the CQCwas troubled.
The Care Quality Commission (CQC)
The CQC was established in April 2009 by merging the Healthcare Commission, the Commission for Social Care Inspection and the Mental Health Act Commission. It would register providers. Uniting health and social services, assessment of local authorities and PCTs might make it possible to bridge the gaps between services. In fact it ensured that inspectors were generalists, often with little knowledge of the services that they were checking. Baroness (Barbara) Young, the first Chair, resigned within a year after conflicts with the Department, having lost confidence in the government’s health check approach to assessing hospital performance. The complexity, overlapping contributions and arguments (both academic and political) about how inspection, regulation and assessment should work, made the issue too hot to handle effectively. A new Chair, Dame Jo Williams, previously of MENCAP, was appointed to carry the work forward. It was soon clear that CQC was a troubled organisation with problems at a senior management level, a large enterprise with a very high workload, and inspectors lacking specialist knowledge in many of the areas of the NHS. Its system examined six groups of issues: client involvement and information; personalised care; treatment and support; safeguarding and safety; suitability of staffing; and the quality and suitability of management. It used quality risk-profiling to identify which providers needed further attention. The CQC registered all 338 NHS Trusts, but made 21 subject to conditions for, among other issues, inadequate infection control. In its first assessments in October 2009, the CQC raised concerns about the 20 Trusts rated ‘weak’ on Quality and a further 27 that had not been higher than ‘fair’ for Quality and Financial Management. At Basildon and Thurrock, there were major problems of hygiene and higher-than-expected death rates. At the Colchester Foundation Trust, the chairman was summarily removed by Monitor. It was “clear that many trusts had significant work to do and a short time in which to do it.”
From January 2010, all Trusts in England were legally bound to be registered with the Commission and, from 2011, this included primary care providers, including GPs and dentists, who had not previously been subject to regulation. The sheer number made this a massive undertaking, not least because the CQC budget fell by a third.76 The CQC named some Trusts (such as Mid Staffordshire and Milton Keynes Hospital) that were told their registration was conditional on improving the safety and quality of their care and maternity services. A further ten Trusts were given only conditional registration. In 2012, the CQC said that more than one in four health and social care providers were failing to meet essential standards of quality and safety.77 The White Paper, Equity and Excellence, and subsequent legislation, removed the CQC’s role of inspecting commissioners to focus solely on the safety and quality of providers. Neither would it have a responsibility for righting problems, which would be for Monitor and NHS England. Working with Monitor, it would operate a joint licensing regime.
The Commission’s role was wider and its staff fewer than its predecessor. It missed some poor providers and its first crisis was at Winterbourne View, a private hostel for 24 residents with severe learning disabilities. It did not react to information from a whistle-blower about serious abuse until a ‘Panorama’ programme in 2011 (that went viral on YouTube) led to its closure and the sentencing of staff – and a Ministerial call for a report into the performance of the CQC and local authorities in the affair. A programme of spot checks began.78 In October 2011, the CQC reported the findings of 100 unannounced inspections of NHS acute hospitals which looked at whether the essential standards of dignity and nutrition were being met on wards caring for older people. It found around half of the hospitals needed to do more to ensure that they were meeting people’s needs – with 20 of the hospitals visited failing to meet essential standards required by law. Shocking examples of bad care were exposed and the CQC called for a system-wide response to combat the failings.79
The cracks in CQC began to show and it came under attack from the Parliamentary Health Committee and National Audit Office for failure to give value for money, and concentrating on registration procedures, reducing the number of inspections and undermining patient safety.80 In 2011, Kay Sheldon, a non-executive director of CQC, warned at a public inquiry that the leadership of CQC was in disarray and public safety was at risk. The chair, Jo Williams, attempted to have Sheldon removed by the Secretary of State but, faced with a challenge to the legality of this, he backed down. Sheldon was later thanked for her contribution.81 With comparatively little publicity, the chair, chief and deputy chief executive left in a substantial clear-out of senior staff.
In 2013, an independent report commissioned by the new chair suggested that top management had suppressed a report on the deaths of mothers and newborns at Barrow in Furness because it showed the CQC’s work to be substandard, and that a cover-up may have taken place.82 The CQC was “apparently more concerned with its image than revealing problems”. The new chair, David Prior, appointed in 2013 and previously chair of the Norfolk & Norwich FT, said that the CQC had not been organised to assess hospital services effectively. Many of the inspectors had no background in health care. Future teams would be larger, professional and under the authority of the new Chief Inspector of Hospitals, Professor Sir Mike Richards, a clinician, who planned a rapid and extensive programme of inspections.
On 23 October 2013, CQC published a list of 161 Trusts, putting them into six risk bands. The Daily Mail and The Guardian summarised the results. “Patients at risk in one in four NHS hospitals”... “based on 150 indicators on the quality, safety and effectiveness of care ... 27% are in the bottom two bands...”83 The data was tentative and no more than an indication of facets of a hospital worth checking, and not on the CQC website. Poor care in one in ten hospital Trusts was, however, noted in the CQC annual report the following month. The effect of such reporting on hospital morale was substantial and why, after many reincarnations of regulators, were over a quarter of hospitals apparently poor? In an interview to acknowledge his first 12 months as Chairman of the CQC, Mr Prior said: “In those hospitals where you would not wish to go, you have a very poor damaged culture where employees feel they can’t raise concerns, where patients are not listened to.” He said the CQC had identified a number of Hospital Trusts as “inadequate”, but highlighted that “Barking Havering and Redbridge is a good example”.
CQC was not in the business of culture improvement, fostering development or encouraging anyone to do better. Its hospital visiting programme now fielded teams of 30–40 people who had spent much time on mastering the details of a Trust they were visiting. Those unimpressed by the efficacy of inspection and regulation thought it was overkill and possibly counterproductive.
The task of inspecting general practice, with surgeries in their thousands was vast. A start was made selecting those that, from statistics, seemed most in need of examination.
Variations in health care
For 40 years, workers in the USA led by Jack Wennberg had found major differences in the provision and usage of services such as hysterectomy and prostate surgery, often unrelated to population need. In ‘effective care’ the benefits outweigh the risks and the right rate of treatment is 100 per cent. In ‘preference sensitive care’ there is more than one generally accepted treatment, informed patient choice is called for, but rates vary extensively because of differences in professional opinion. ‘Supply sensitive care’ depends more on the capacity of local facilities than on clinical need.84 The Dartmouth Health Atlas had showed conditions where the rate of surgery differed greatly. The idea of an atlas was taken up in England in 2010, overseen by Sir Muir Gray and Philip DaSilva, who acknowledged the ‘inspirational publication’ of Wennberg’s atlas and his vision in first charting this territory.85
The English version was created in 2010, and later revised, within the Department of Health’s quality, innovation, productivity and prevention programme (QIPP).86 The NHS Atlas of Variation in Healthcare showed dramatic differences in wellbeing, health outcomes, spending and service provision across England, much inexplicable by health need. Some variations highlighted shortcomings in the quality and value of services for underprovision is as much a problem as overprovision. A function of the atlas was to encourage commissioners to look at the unwarranted variations, some of which seemed examples of Julian Tudor Hart’s “inverse care law” – the greater the need, the poorer the access. Thirty-four maps covered different conditions, for example, asthma, and amputation for diabetes. There was more than a tenfold variation in the proportion of high-risk transient ischaemic heart attack cases treated within 24 hours.
The geographical pattern of mortality in Great Britain over the previous 25 years was also mapped to show how likely death was, dependant on location. The Grim Reaper’s Road Map: An Atlas of Mortality in Britain showed how people’s deaths are affected by where they lived, how much money they had, the type of work they did and their life style.87 Maps showed the chance of dying from a particular cause in a particular place compared to the national average chance, having standardised by age and sex in each area. The maps showed deaths from a range of causes, including heart attack, cancer, murder, electrocution and death during surgery. Across much of the south of England outside London, and in a few isolated enclaves of prosperity in the north, Wales and Scotland, people’s chances of dying each year had been up to 30 per cent lower than the average since 1981. What caused most of the variations were not genetic factors, said the authors, but environmental issues and whether we smoke, drink and exercise. Death rates are higher where people were poorer. Internal migration was another key factor, making different parts of Britain increasingly home to either the poor or the rich.
Hospital standardised mortality ratios (HSMRs)
One tool used to identify hospitals where care might be poor was standardised hospital mortality ratios (HSMRs). A concept developed earlier in the USA, the indicators had critics but were welcomed by patient organisations. The UK HSMR was derived from Jarman’s work dating back to 1993 with Dr Foster, an independent organisation collecting data from hospitals on a voluntary basis. It was a statistical calculation that measured the overall rate of deaths within a hospital or Trust compared with a national average. The HSMR focused on the medical conditions associated with 80 per cent – not all – of deaths in hospitals. It did not adjust for the many patients admitted specifically to provide care near the end of life, and the results were increasingly criticised because of variations in coding practice and the extent to which multiple morbidities, which increased death rates, might or might not be coded. Unjust criticism of a hospital could destroy morale and create inappropriate criticisms. Some findings were of great interest, for example, Dr Foster showed that mortality rose slightly in the first week of August when new doctors took up their posts; a similar effect was seen in the USA in July when the same thing happened. If HSMRs were not used to make heroes or villains, they were perhaps one of the best measures we had. Media comment made Dr Foster’s data a matter of public interest.88
The Department of Health and regulators became engulfed in the row over the methodology because the ratings often seemed inconsistent with Trusts’ performance. Sometimes a low rate was associated with clear clinical shortcomings. Sometimes it was not. In the USA, the National Quality Forum was also seeking measures of hospital quality. A Massachusetts study compared the results from four different, commercial, hospital-wide mortality “products” including Dr Foster. They were each given exactly the same database. The results from the four vendors differed markedly, and in some cases hospitals identified as above average performers by one commercial system were classified as below average by others, and vice versa. The study concluded that “without clear consensus on a methodology, public release of hospital mortality results can potentially create patient distrust and confusion among consumers.”89 There was an increasing number of organisations in the quality assessment field and after a tendering process in 2010 during which eight organisations submitted bids, the contract to provide HSMRs passed to market research company, IMS, “a premier source of global pharmaceutical marketing intelligence”.
To resolve the concern that different systems produced different results, the NHS Medical Director, Sir Bruce Keogh, established a group to agree a method for calculating hospital mortalities in 2010. It suggested a new measure, the Summary Hospital-Level Mortality Indicator (SHMI) that covered death relating to all admitted patients that occur in all settings – that is, including those occurring in hospital and 30 days post-discharge, and adjusted as far as possible with Hospital Episode Statistics (HES) data for factors outside a hospital’s control that might impact on hospital mortality rates, and applied to all NHS Acute Trusts except specialist hospitals. There might be mitigating factors – in Hull, for example, hospice facilities were meagre and more people might therefore die in hospital. But assessments needed to be made, and to be improved. A start was made in 2014 in the publication on the NHS Choices website of mortality data of individual surgeons.
Professional regulation
The Council for Healthcare Regulatory Excellence became the Professional Standards Authority for Health and Social Care in 2012, having acquired oversight of the regulation of social workers in England. In 2009, the General Medical Council introduced the licence to practice, required for all practising UK doctors in addition to their registration. Licensing was the first step towards the introduction of revalidation to give patients assurance that doctors were up to date and fit to practise. Revalidation was likely to include appraisals, assessments and specialty standards.
The National Institute for Health and Clinical Excellence (NICE)
In 2009, NICE reached ten years of age and kept going. Controversial from the outset, its survival was to be celebrated and it was one of the most successful pieces of policy-making, shielding politicians from many really difficult decisions, and emulated in many other countries.
Questions remained: was the threshold for deciding which drugs were cost-effective enough to use too low or too high? It was certainly arbitrary. Was treating an older person inherently less economic than treating a younger one? The Department of Health believed NICE should take “wider societal benefit” into account when considering whether to pay for a drug.90 NICE demurred – it was not ageist. It did not stop the use of less cost-effective interventions already in use; it could not assess the whole of medicine. How should drugs be handled when companies chose to submit no evidence? In the absence of an inquiry by NICE, they continued to be used.
Decisions might be revised as happened with ranibizumab (Lucentis) for age-related wet macular degeneration. In 2008, draft guidance by NICE was criticised by oncologists for saying that four drugs for rarer cancers, which could prolong life but not cure, should be denied on cost-effectiveness grounds. The oncologists believed that any restriction of prescribing on the grounds of cost was reprehensible and the Conservative opposition agreed. Others felt that there had to be some limit to the costs the NHS was expected to pick up. NICE revised its appraisal procedure and some, but not all, were approved. Kadcyla, which, on average, added six months of life to women dying of an aggressive form of breast cancer, might not be approved at its cost of £90,000 per patient. Of 102 uses of drugs for cancer examined by NICE between 2002–2010, 73 per cent were approved. Of 372 assessments of all drugs, 83 per cent were accepted.91
The Chair of NICE, Sir Michael Rawlins, wrote:
It really is time that some of my clinical colleagues woke up to the realities confronting all health care systems. An ageing society, technological advances and public expectations are placing demands that all countries are struggling to meet. Countries do not have infinite sums of money to spend on health and the amount they can afford is largely governed by their wealth as reflected by their gross domestic products. The debate is not about whether – but how – health care budgets can be most fairly shared out among a country’s citizenry.92
He thought that the prices charged by drug companies were excessive. Others – in support of the pharmaceutical industry – replied with some justification that only an industry with the profit incentive would produce new drugs, quoting the regular appearance of drugs for AIDS.
NICE was caught, inevitably, in media storms. Firm implementation of national guidelines might ensure a consistent deal for patients across England, if not in Scotland, Wales and Northern Ireland. NICE had to take account of all who depended on the NHS (not just patients suitable for treatment by the drugs it considered).
NICE was often slow to make an assessment. The Labour government proposed a faster system for referring drugs and health care technologies to NICE, a new NICE committee to increase its capacity to assess new drugs, more ‘horizon scanning’ to help identify new drugs and issues early; and guidance for PCTs on how to deal with requests for drugs not yet assessed by NICE. In 2010 the Conservative/LibDem government proposed a special £200 million Cancer Drugs Fund to pay for significant but expensive cancer drugs. Andrew Lansley said, “It is unacceptable that we should be one of the leading countries in Western Europe for cancer research ... yet sometimes it’s our patients ... who find that they don’t have access to the latest new cancer medicines.” This fund created the controversial situation of two parallel assessments, proved too small in any case and, in 2016, it was integrated into the NICE system, with NICE making judgements on cost effectiveness, and approving drugs for a limited number of patients to provide better data.
Evidence-based quality standards programme
In 2009 NICE was commissioned by the Department of Health to manage the process of developing independent quality standards, a consistent set of measures which might be used in commissioning and inspection. Topics were selected by the National Quality Board, created in 2009. The first of 150 standards dealt with the quality of care in stroke, venous embolism and dementia. For example, it said that patients who had had a stroke should be offered at least 45 minutes of active therapy five days a week. NICE expanded into a new field – nutrition. It recommended that, to reduce deaths from cardiovascular disease, attempts should be made to reduce the nation’s consumption of salt, saturated fats and trans fats.
Medical progress
In the 1950s, Professor Sir Max Rosenheim, at University College Hospital (UCH), jokingly defined a fit person as one who had been inadequately investigated. A long-standing concern about ‘medicalisation’ led to the belief that the definition of common conditions had been broadened so much that the entire elderly population had at least one chronic disease. The diagnosis of prehypertension, irritable bowel syndrome, attention deficit hyperactivity disorder (ADHD), bipolar disorder, gestational diabetes, grieving and depression and other conditions was widened so people with mild problems at modest risk were exposed to the harms and costs of treatment of little or no benefit. New diagnoses could be as dangerous as new drugs. Those considering the definition of disease often had significant links with the pharmaceutical industry and, loath to miss potential patients, erred on the side of treatment. In the USA in particular there were many doctors with major financial income from ‘big pharma.’ The Food and Drug Administration (FDA) discouraged them from taking part in advisory panels on the approval of drugs. In 2016 the Academy of Royal Colleges issued a list of 40 interventions that it felt were unnecessary; procedures that were of little or no benefit to patients.
Long-term conditions
According to the Parliamentary Health Committee Report in July 2014, 15 million people had one or more long-term illnesses such as diabetes. Care for long-term conditions accounted for 55 per cent of GP appointments, 68 per cent of outpatient and A&E appointments, and 77 per cent of inpatient bed days. This presented a major financial challenge: care facilities in the community needed to be built up, and transfer from hospital to the community would not necessarily save money.
Public health
The goal of the World Health Organization (WHO) declaration in 1978 on Healthcare for All 2000 had not been achieved. In 2008 a new report appeared from the same city, Alma Ata now known as Almaty, Now More than Ever.93 It said that better outcomes for the population at lower cost were achieved in systems that distributed resources according to health care needs, eliminated co-payments, assumed responsibility for funding and provided a broad range of services within primary care. While Britain appeared second only to Canada in the proportion of resources devoted to prevention and public health, from 2014 the money spent fell, subsequent to the transfer of public health functions to local authorities.
Health inequalities
The persistence of widespread inequalities in health, even in a system with two generations of universal free access, is a great unsolved mystery of medicine. Alan Johnson, when Secretary of State, made the narrowing of ‘health inequalities’ a priority. Health Inequalities: Progress and Next Steps was published in 2008, supported by Sir Michael Marmot.94 He described the drop in life expectancy by one year at every two tube stations going east on the Jubilee line from Westminster to Canning Town. While the health of the poorest had improved significantly, the health gap remained. National targets were set to reduce inequalities in health outcomes by 10 per cent, as measured by infant mortality and life expectancy at birth by 2010. There would be restriction of TV advertising before 9pm of high-calorie junk foods. Primary health care services would include health education on life style. Reliance was sometimes placed on self-regulation by industry in the hope that manufacturers would reduce the sugar and salt content of their products. PCTs in the more deprived areas would receive extra money to pilot such initiatives as health trainers.
In February 2009, the Parliamentary Health Committee reported that, while health in the UK was improving, over the last ten years, health inequalities between the social classes had widened – by 4 per cent amongst men and by 11 per cent amongst women.95 The NHS atlas of variations in health care, published online, illustrated the changes in life-expectancy graphically.96
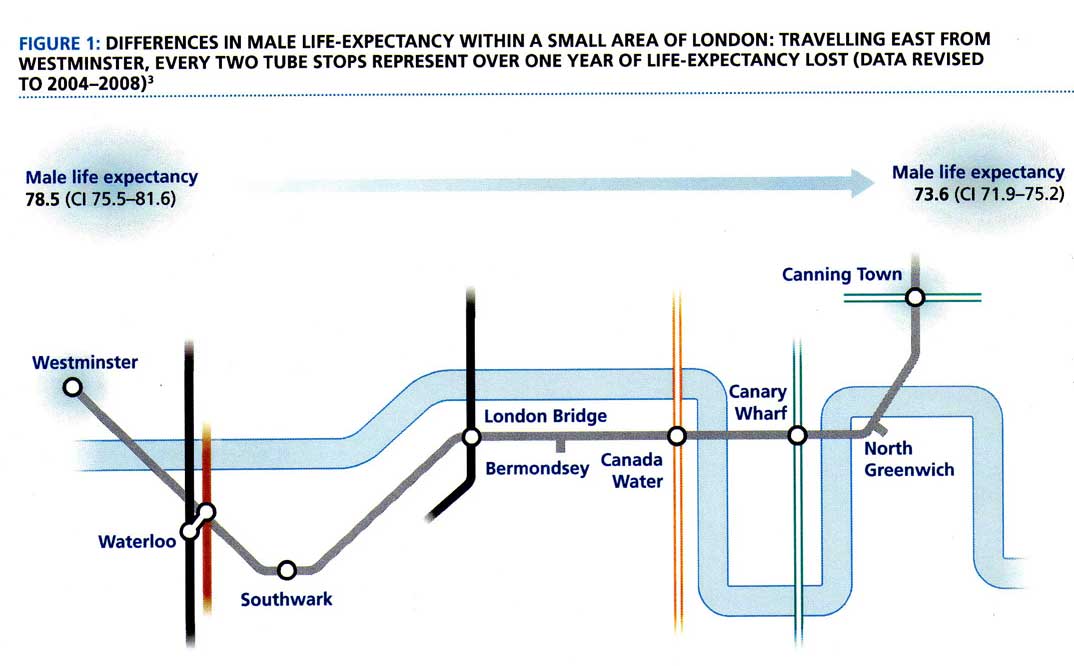
The Marmot Review
A further review of health inequalities was announced in November 2008 by Gordon Brown, the Prime Minister, and commissioned from Professor Sir Michael Marmot to help government’s health inequalities strategies and set objectives for future action in England.97 Examining existing work, Fair Society, Healthy Lives was published in February 2010 and was an analysis of the situation in England. The review stressed the importance of the early years of life, and early child development programmes, safe neighbourhoods and decent housing. All public policy, not just health policy, should reflect social justice, health and sustainability. It made a number of policy recommendations.98 The Guardian said: “The Marmot report has made it clear – for better social wellbeing we must slash disparities in education, income and health.” The response to the Marmot Review was published by the coalition Conservative/LibDem government in a White Paper, in November 2010. It contained few surprises but was welcomed by Marmot.99 The long document presented the customary facts about health inequalities, and the usual targets for intervention. It said that government was radically shifting power to local communities, enabling them to improve health throughout people’s lives, reduce inequalities and focus on the needs of the local population. Reliance was placed upon Public Health England, an executive agency of the Department of Health, to act where possible. Public health responsibilities moved to local government in April 2013, authorities appointed a director of public health, accountable to them and advising on commissioning. The Department set targets for the reduction of deaths in the major groups such as cancer, circulatory diseases, suicide and accidents. Sir Michael was appointed as director of a new University College London (UCL) Institute of Health Equity, established with departmental funding in 2011, that aimed to reduce health inequalities through action on the social determinants. In 2018, government’s commitment to preventive medicine was reiterated in Healthy Lives, Healthy People – Our Strategy for Public Health in England. There was little that was new.
Health promotion and health screening
A ‘Mediterranean diet’ had consistently been shown to be associated with longevity. The dominant components seemed to be moderate consumption of alcohol, low meat consumption, and a high consumption of vegetables, fruit, nuts, olive oil and legumes. Faced with the ‘epidemic of obesity’ and wishing to reduce health inequalities, the use of financial incentives to achieve healthy behaviour was high on the agenda. Disincentives in the form of alcohol and tobacco tax were known to reduce consumption. The effect of positive incentives was less clear cut. In 2009, government launched Change4Life, a ‘society-wide movement’ aiming to prevent people from becoming overweight by encouraging them to make changes to their diet and levels of activity. Other campaigns related to the avoidance of fizzy drinks containing high levels of sugar, and the use of sun beds by those under 18, in the light of the rising number of cases of skin cancer.
In 2008, Gordon Brown, when Prime Minister, had announced a programme of preventative health checks. These began in 2013 as check-ups for those aged 40–74 every five years covering life style, body mass index, blood pressure and cholesterol concentration. Commissioned by the local authorities, now with public health responsibilities, they were introduced on the principle that they might help, although they were neither based on substantial evidence of benefit, nor to be subjected to effective assessment. The evidence pointed the other way. Screening will cause harm in some people. Repeated randomised trials showed not a trace of an effect on mortality.100
Obesity, food, alcohol and health
What should one eat? The incidence of obesity was increasing, type 2 diabetes as well, and ‘authoritative recommendations’ followed. Not all were soundly based and the food industry sometimes had influenced ‘research’ and the presentation of data. Perhaps saturated fats and cholesterol-containing eggs were not really so lethal? Were we eating too much carbohydrate and, in particular, sugar? Some foods – for example, processed foods and red meat – seemed associated with cancer, but was this truly a causal relationship? How great was the increased risk and what, if anything, was undoubtedly ‘safe’ to eat?
Alcohol misuse posed a huge clinical and public health problem throughout Europe. Those who had campaigned against smoking had a new target. In the UK, alcohol consumption had risen at the same time as its costs, in real terms, had steadily fallen. In 2009, England’s Chief Medical Officer (CMO), Liam Donaldson, had called for a minimum price for alcohol. The BMA, the Royal College of Physicians (RCP), and the Faculty of Public Health added their voices to the demand, believing that the serious effects on health and society could best be mitigated through legislation on price and marketing. In 2010, NICE also argued for a minimum price per unit of alcohol to reduce consumption. Scotland passed legislation but delayed its implementation because of legal challenges. David Cameron, as Prime Minister, had supported the proposal, but after intensive lobbying by the alcohol industry, government changed its policy on the grounds that there was not enough evidence that its introduction would reduce the harm associated with problem drinking without penalising people who drank responsibly.101
The drug treatment of disease
Fewer new drugs were being developed and, to encourage research and to make the country a more attractive base for the pharmaceutical industry, it was hoped to make anonymised information from the NHS (care.data) available as a research resource. Drug therapy was converting fatal diseases into chronic ones, to be controlled if not cured. A new chapter was opening for medicine based on the molecular basis of drug activity, cancer probably being in the lead, although other specialties were following. Most drugs had emerged before this and results were not always consistent, for example, only a quarter of patients with breast cancer benefited from Herceptin. The better the knowledge of genetics, the better therapy might be. Increasingly, new drugs were the result of genetics. Monoclonal antibodies were more and more used in treatment and, by 2012, over 20 were in use for conditions varying from cancer, to autoimmune diseases, to extremely rare inherited disorders. They were eye-wateringly expensive and a major source of income for drug companies, but might be useful in diseases such as multiple sclerosis, previously untreatable. Drugs that hit a particular DNA segment might be effective in several diseases. Biological markers of effectiveness were required, molecular level signatures of response, so that treatment could be personalised and money was not wasted on people who were not benefiting. If non-responders could be identified, some of the rising costs could be avoided.
Greater access to medicines was possible by increasing the range of trained professionals allowed to prescribe them. Out of 690,000 nurses in 2009, 40,000 could prescribe, the majority in general practice. The process had gone smoothly, nurses being cautious, many having ‘supplementary’ rights to prescribe within a care management plan agreed in advance with a doctor. ‘Independent’ prescribers could prescribe any medicine for any condition that fell within their area of competence. Where nurses were leading, other professions were following – for example, pharmacists. Some who met specific criteria could obtain particular medicines automatically.
More prescription drugs became available over the counter if considered safe. Sixty were reclassified from ‘prescription only’ to ‘pharmacy only’, for example, simvastatin, (statin), griseofulvin (antifungal) and hydrocortisone and nystatin ointment.
Withdrawal of drugs for safety reasons
Drug warnings became common. In 2010 alone there was a caution that off-label use of quinine for leg cramps could result in serious and life-threatening effects on the blood. Long-acting beta agonists were associated with an increased risk of muscle destruction; the opioid tramadol was linked to increased suicide risk; bisphosphonates used to treat osteoporosis had a possible increased risk for atypical femur fractures; and tigecycline was linked to an increased risk of death in patients with certain severe infections. In 2015, the drug for epilepsy, Epilim (sodium valproate), if taken in pregnancy was shown to be associated with delayed walking, speech, memory and language skills. Thousands of pregnancies had been affected, and an inquiry was opened in 2017.
Two of the three drugs released earlier for the drug treatment of obesity had not lived up to their promise and were withdrawn because of clinical trial data pointing to an increased risk of stroke and heart attack. Roughly 100,000 people in the USA were taking sibutramine at the time.
The diabetes drug rosiglitazone (Avandia) for type 2 diabetes had been licensed ten years previously and lowered glycated haemoglobin. Controlling blood sugar was assumed to mean that the vascular complications of diabetes would be reduced. There had been only limited evidence of its safety and, over time, it appeared to increase rather than reduce the incidence of heart disease. The BMJ thought it should never have been licensed and should now be withdrawn, which it soon was. The information needed for licensing was likely to be reviewed, with a greater requirement for robust evidence on benefits and harms. Some drug companies, when presenting the results of clinical trials to regulators, might suppress information from those that showed no benefit – or indeed harmful effects. Meta-studies might mislead if, as had sometimes been the case, much of the information available was not presented.
Top-up drugs
Some new drugs were costly and extended the life of those with an incurable disease, but did not affect the outcome. NICE, applying the criteria of cost effectiveness, might not approve them for NHS use. Patients faced with death which might be delayed by therapy not available within the NHS sometimes bought them personally, perhaps at the cost of thousands of pounds. However, this might debar them from receiving normal NHS care at the same time, and protests led the Secretary of State to commission an inquiry. In November 2008, Professor Mike Richards recommended that the government, NICE and the pharmaceutical industry should act to ensure that more drugs were available for NHS patients on the NHS, but that those few that still wished to buy additional private care should not lose their entitlement to NHS care if the private element could be delivered separately from NHS care. The speed with which such drugs were referred for assessment by NICE should also be increased.
Radiology and diagnostic imaging
The technology available to radiologists had changed dramatically with IT, affordable high-performance computers, digital imaging and picture archiving and communication systems (PACTS). As a result, imaging and interpretation were no longer confined to one site. The demand for imaging grew steadily as increasingly every field of medicine and surgery depended on imaging. For example, computed tomography (CT) coronary angiography became standard. As a result, there was a shortage of doctors trained to interpret scans. Remote assessment, already frequent in the USA, became more prevalent in the UK.102 Complex imaging procedures were frequently required in accident departments around the clock. Outsourcing of interpretation was one way of dealing with increased demand when there was a shortage of radiologists. Some English hospitals outsourced part of their work into Europe, as far away as Barcelona. This had its problems. Access to other test results or previous images was seldom possible, nor the easy communication with other specialties.
The steady improvement of imaging and nuclear medicine equipment provided better images and increasingly smaller radiation doses. The combination of CT and positron emission (PET) scanning improved the diagnosis of heart disease and cancer. As the quality of imaging improved, unexpected findings were increasingly encountered, often of clinical relevance and unrelated to the purpose of the imaging. Magnetic resonance imaging (MRI) scans were usually requested to solve a specific clinical problem, but other small lesions, such as meningiomas, might be found. A new imaging system, laser-based optical tomography, provided a new way of looking at the skin to a depth of 1mm, particularly relevant in ophthalmology.
Cheap portable ultrasound scanners were changing the way doctors examined and diagnosed their patients. The results of treatment might be assessed by repeated imaging; the array of imaging tests increased. Over ten years, the use of CT scans had doubled. However, radiological investigations, particularly if they were repeated, or in pregnant women or children, could lead cumulatively to a high dose and increase the risk of cancer. One estimate was that such radiation might be responsible for 2,000 cancers a year in the UK.
Infectious disease and Immunisation
Drug resistance and anti-bacterials
From the 1930s to 1960s, 14 classes of antibiotics were introduced. In the past 30 years, only two novel classes of antibiotics had entered the market – oxazolidinones and cyclic lipopeptides – both used against Gram-positive bacterial infections. No new drugs against Gram-negative bacteria such as E. coli and K. pneumoniae had been marketed. Few were now under development – the profit on drugs used once and effectively, was lower than those for chronic conditions. The resurgence of life-threatening resistant strains of bacteria was a crisis waiting to happen, prompting leading bacteriologists to urge government, charities and industry to invest in research in this field.103 Were resistant strains to become dominant, medicine would be set back decades. Many procedures, for example, transplants and hip surgery, depended on the ability to control infections. Some procedures would be highly dangerous if this control was weakened. MRSA first appeared in 1961 (methicillin was developed in 1951) but it was several decades before it became a problem. In 1992, the number of strains that were resistant in hospital practice reached some 50 per cent. Now similar strains became more common in the community, in young fit people, sometimes with sports and soft tissue injury. Clinicians outside hospitals had to be aware of this increasing hazard. Resistant strains included, Streptococcus pneumonia, Staphylococcus aureus, Escherichia coli, Enterococcus faecalis, Enterococcus faecium, Klebsiella pneumonia and Pseudomonas aeuruginosa.
Septic shock was a major cause of death and one of the main reasons for admission to hospital intensive care units. Rapid recognition and immediate treatment was crucial to survival. The national imposition of systematic cleaning of hospitals and wards was associated with a reduction in the number of cases of MRSA and C. difficile. From 2008 onwards a new threat emerged, New Delhi metallo-lactamase 1 or NDM-1. This was an enzyme that could live in different bacteria, which were then resistant to most antibiotics. The Lancet reported 50 cases in the UK (and many more in India and Pakistan), including E. Coli and Klebsiella pneumoniae, with some deaths.104 NDM-1 was becoming more common in Bangladesh, India and Pakistan, and was starting to be imported back to Britain in patients returning from these countries. The main antibiotics for the treatment of gram-negative infections, â-lactams, fluoroquinolones and aminoglycosides - were no longer useful in these cases.
Tuberculosis
Easy travel and migration led to the re-emergence of tuberculosis as a public health problem. In 2009, 9,040 cases of active disease were notified, a 75 per cent increase over 20 years. Most occurred in people born outside the UK, often several years after arrival. Patients often came from countries with a high prevalence of tuberculosis, and indeed of multiple drug resistance. Often presenting late and in the homeless, alcoholics, those on drugs such as crack cocaine, in prison or with HIV, these were groups difficult to reach, poor at adhering to treatment and were often highly infectious. London and other conurbations were witnessing a vast increase in cases and new strategies were tried. Targeted screening with modern mass radiographic systems supported by better tests for infectivity picked up the disease earlier and gene tests made it possible to determine drug sensitivity rapidly. Regular treatment taken under observation and better follow-up where patients lived increased compliance and the success rate.
AIDS
Annual numbers of HIV diagnoses in the UK doubled between 2000 and 2005 and had remained above 7,000 in each year until 2009 then falling slightly to 6,360 in 2012. Three-quarters of new cases were in men, evenly split between heterosexual contacts and men sleeping with men. About one pregnant woman out of 450 was HIV positive, more in sub-Saharan immigrants. However, highly active anti-retroviral therapies (HAARTs) delayed the progression of HIV to AIDS, reducing HIV-associated morbidity and mortality.105 It was estimated that there were some 100,000 cases of infection in the UK, 20 per cent undiagnosed, and late diagnosis was a major cause of treatment failure. “Get tested” was the message and, from 2014, it was legal to buy a blood or saliva test over the counter.
By the beginning of the decade, there were more than 25 antiviral drugs from six therapeutic classes available for the treatment of AIDS. In developed countries multiple drug regimes were normal and most people who took medication achieved durable viral suppression. A new issue emerged – an increased incidence of disease in long-term survivors. Classic AIDS-related conditions were becoming less common but, compared with a normal population, ‘non-AIDS related’ conditions were more prevalent. Heart disease, cancer and liver disease and conditions related to ageing appeared most likely when treatment did not restore cell counts to the normal range. The care of patients with AIDS was becoming more complex.
In the 1970s, many haemophiliacs had been infected by HIV as a result of substandard blood products. Lord Archer had reported on this in 2008 and, in May 2009, the government expressed regret and increased financial compensation.
Scarlet fever
A surprising return of scarlet fever was seen in 2014, with over 5,000 cases in six months.
BSE
The number of new cases of variant Creuztfeldt-Jakob disease (vCJD) continued to decline, with one in 2008, three in 2009 and 2010, and one in 2013, with a total of 177 proven or probable deaths by 2014. However, it was estimated that one in 2,000 people carried vCJD in their blood and might either later develop the disease or transmit it through blood products.
Tropical diseases and Ebola
Even though malaria is not endemic in the UK, there were well over 1,000 cases annually in those returning to or arriving in the UK, mostly in people who had travelled to or from African countries, but a substantial number in people who had travelled to or from Asia, Far East, and southeast Asia.
Ebola returned as a major problem in 2014, with a massive outbreak in Liberia, Sierra Leone and Guinea. Vaccine development was pushed forward rapidly. Many health care workers developed the infection, and some died. By the time, in 2016, that WHO declared the epidemic over, at least 11,000 had died. WHO was accused of slowness in its response.
Zitka virus, carried by mosquitos and first identified in monkeys in Uganda in the 1940s, and which crossed into humans in Nigeria in 1954, began to spread more widely in 2016. It was linked with microcephaly following infection in pregnant women, and with the paralytic Guillain-Barré syndrome – 4,000 children in Brazil were affected and cases were reported in the Caribbean and Hawaii. The Centers for Disease Control and Prevention (CDC) in Atlanta warned pregnant women not to travel to 22 countries, mainly in the Caribbean, and cases were reported in British tourists.
Swine Flu
The risk of pandemic influenza had led to warnings of disaster for years, though neither severe acute respiratory syndrome (SARS) nor the small outbreaks of ‘bird flu’ in the Far East had affected Europe significantly. The threat of an epidemic had been the subject of planning and there was concern about the ability of the NHS to keep running at a time of mass illness which would affect staff. In 2009, an outbreak of Swine flu (H1N1) with many deaths in Mexico created worldwide anxiety. CDC Atlanta said it was probably impossible to contain it and its advice was designed to slow the spread of the virus. Some countries reacted incoherently, for example, slaughtering pigs en masse. Within weeks, dozens of countries had cases, and while some were severely affected, mostly cases were mild in nature. Indeed the normal victims of flu, the over 65s, were less likely to contract the disease because of pre-existing immunity. The US Federal Government and manufacturers rapidly began to develop a number of vaccines against the novel H1N1 flu virus. In the UK, 44 million doses of the newly developed vaccine were eventually purchased (more were initially ordered) and in October 2009 vaccination began. The take-up was understandably low. Rarely one particular vaccine, GSK’s Pandemrix, used in 47 countries but not the USA where regulators were wary of adjuvanted vaccines, produced problems. In a number of countries, narcolepsy was induced in one in 16,000 of those receiving it. There were 200 cases in Sweden that had been highly effective in its vaccination campaign. Narcolepsy could follow swine flu itself, but could also follow vaccination. Part of a surface protein on the pandemic virus looks very similar to part of a brain protein that helps keep people awake. When a person’s immune system learns to recognise and fight the virus, it mistakes the brain protein for an invader, too. Government accepted the link and compensation claims were settled.
In England antivirals such as Tamiflu (oseltamivir) were initially used prophylactically for contacts but this strategy of containment failed and the number of cases slowly increased, mostly in the young. Deaths occurred, particularly in those with lowered resistance because of other diseases. Pregnant women and young children seemed particularly at risk, but while the number of cases was much the same as those in a “normal” year, deaths did occur. In July 2009, the CMO, Liam Donaldson, spoke of a worst case scenario of 65,000 deaths. Fuelled by government and the media, public anxiety and the pressures on primary care grew. In July 2009, 100,000 cases were recorded in a week. A National Pandemic Flu Service was launched (GPs were taken out of the equation) and a phone line and website were established – less than one in 20 callers actually had the disease.
The service also made antiviral drugs available directly to the public if they gave a history suggestive of infection. Comparatively few picked up the drugs for which they had asked. A revised assessment by the Cochrane collaboration threw doubt on the ability of oseltamivir to reduce complications in otherwise healthy adults or had any effect on stopping people infecting others. Serious illness other than influenza might be misdiagnosed and some undoubtedly suffered because diagnosis of their real illness was delayed. The drug had its own side-effects, some serious.
While the Secretary of State, Andy Burnham, said England had come through the epidemic because of the strength of plans, this was clearly not so. Nobody seemed to have thought of a pandemic so mild that it would cost fewer lives than normal seasonal flu. By January 2010, the weekly case rate was below 5,000. Only a third of the vaccine purchased was used, and attempts were made to dispose of the surplus. Post-mortems began; had public health doctors over-reacted? Had the pharmaceutical industry created a panic to increase the sales of their products? Had money been wasted? Would anyone believe predictions again? It was hard to say any one decision was wrong, but once the concern was there, one step followed another with grim inevitability.106
The Social, Health and Family Affairs Committee of the Council of Europe, reporting in June 2010, criticised WHO, national governments and the EU agencies for the handling of the epidemic, “a pandemic that never was” and a waste of large sums of public money. There had been lack of transparency about how decisions had been taken and possible conflicts of interest. Nigel Hawkes said that “money spent in stockpiling antivirals with hypothetical effectiveness against a hypothetical pandemic is not available for health care, or for education or for any other important human need”. A government-commissioned review found the swine flu pandemic cost Britain more than £1.2 billion, despite being much less severe than feared. The actual death toll during the outbreak was 457, not 65,000. Some in public health believed that the response had been “proportionate and effective”, though not all agreed.
The following year, 2010/11, influenza appeared and swine flu infections were again apparent. Though the death rate was not high, the disease affected an unusually high proportion of young people. The facilities for extracorporeal membrane ventilation were increased, to cover the number of people in intensive care with breathing problems. The government also purchased more antivirals as existing stock went out of date. Experts differed: given the possibility that the next epidemic might be worse, was it better to have no reserves of antivirals, when we have nothing else available with which to treat a novel pandemic flu virus? Data from the 2009 pandemic showed that antivirals did save lives. It seemed sensible to have an adequate supply.
E. Coli
A significant outbreak of Escherichia coli 0157, in a Surrey farm open to the public, where animals could be fed and petted, occurred in September 2009. Ninety-three people were involved, 76 children under ten. Some became seriously ill, requiring renal dialysis. An enquiry concluded that laboratory closure over a bank holiday weekend, incorrect advice, and delay in restricting access to the farm – fundamental failings in the handling of the outbreak – increased the number of cases. Found on almost 40 per cent of cattle farms, risks might be minimised but could not be eliminated.
A far more serious outbreak occurred in Germany in May 2011, difficult to trace but ultimately linked to bean sprouts from an organic farm in Lower Saxony. More than 4,100 people in 12 countries, including France and the UK were infected, all of whom had travelled to Germany, with 49 deaths. The new strain, enterohaemorrhagic E. coli (EHEC) was an aggressive hybrid toxic to humans and not previously linked to food poisoning. In over 700 patients, it led to haemolytic-uraemic syndrome, with kidney failure. Instead of affecting many children, a lot of patients were adult women, well educated, and food conscious. Restaurants were part of the chain.
Immunisation
The false reports of harmful results of immunisation with measles, mumps and rubella (MMR) vaccine had led to many children being unprotected. A substantial outbreak of measles in Wales in 2013 (some 1,000 cases) where many children (then in their early teens) had not been protected, led to substantial campaigns, both in Wales and elsewhere to control the disease.
The first trial of a vaccine against human papilloma virus (HPV), the cause of cervical cancer, was conducted in 2002. As it was effective only before infection, and the majority of women were infected within nine months of starting sexual activity, it had to be administered early. It was offered to 12–13-year-old girls from September 2008, and soon 90 per cent had had their first of three vaccinations. Though costly, it was decided to cover 13–17-year-old girls as well. A slow-growing cancer, it would be 30 years before the effect was likely to show on the death rate.
Immunisation using an oral vaccine against rotavirus, a cause of acute diarrhoea and many hospital admissions in infancy, was added to the childhood programme in 2013. An oral attenuated live vaccine, it was given between two and three months of age. The coverage of immunisation in childhood continued to expand, with addition of Meningitis B (HiB 2015) and Hepatitis B (2017). A multivalent vaccine covering Hepatitis W was recommended for those going to university.
Surgery
Changing demand for surgical procedures led to new specialties. Bariatric surgery increased rapidly so that, by 2014, some 8,000 such operations were being carried out annually, mainly in the NHS. The ‘epidemic’ of obesity, junk foods and inadequate inadequate activity, was blamed. Those operated on had for years tried to lose weight but it was said that some might even eat to gain a weight that would qualify for health service care under the guidelines. The incidence of type 2 diabetes, heart disease, and health generally improved after surgery and the operation paid for itself in reduced costs to the NHS over a few years.
Cosmetic surgery was increasing rapidly – 90 per cent in women and often in the private sector as a life style choice. There was little regulation and a grey area between cosmetic surgery by fully trained professionals, and cosmetic procedures undertaken in beauty salons where staff might have little training and use injectable fillers of uncertain origin. The revelation that a major producer of breast implants had used substandard silicone gel in prostheses with a high rupture rate led to calls for regulation, better assessment of the competence of those undertaking procedures and record keeping. A review led by Professor Sir Bruce Keogh, the medical director of NHS England, recommended better regulation, better training and proper redress if things went wrong, recommendations that were largely accepted.107
Minimal access surgery
Two new minimal access techniques were under development. Natural orifice endoscopy used a natural cavity such as the rectum or vagina for access, avoiding the need for an external scar. Single port laparoscopy involved, instead of several stab incisions providing surgical access, only one at the umbilicus, again avoiding scaring. Appendicectomy, cholecystectomy and even partial colostomy were possible in this way which its protagonists thought was safe in well-trained hands, virtually scar less, and of reasonable cost.
Organ transplantation
While there were more donors and survivors than ever before, long-term survival was increasing and waiting lists for kidney transplants were falling, and the demand for transplants continued to exceed the supply of organs. With a waiting list of 10,000, three people died in the UK every day because of the lack of a suitable organ. NHS Blood and Transplant accepted the growing practice of offering patients organs that were less than ideal, for example lungs from heavy smokers or livers from people who had died in their seventies, the choice being death while waiting or a high chance of survival.
The scope of tissue transplantation was widening to include the uterus – in 2014 a baby was born in Sweden successfully after transplantation – and the gastrointestinal tract. Over the previous ten years, intestinal transplants had moved from an experimental procedure where failure was almost to be expected, to a more regular procedure, usually performed for people with a short gut as a result of Crohn’s disease or the removal of tumours. The USA, Germany and France were in the lead. In intestinal failure, the intestines can’t digest food or absorb the fluids, electrolytes and nutrients essential for life. Patients with life-threatening complications from total parenteral nutrition (nutrition into a vein) such as liver injury could now be considered for gut transplantation with or without other organs such as the pancreas and liver, with a fair chance of five-year survival, and it was the only long-term option for those with intestinal failure. A pioneering biomedical engineering operation allowed the implantation of tissue grown outside the body. After many years of careful laboratory, immunological and animal work, a joint team from Bristol, Spain and Italy collaborated in the removal of a main bronchus largely blocked by tuberculosis that had led to lung collapse, and its replacement with a new piece without the need to use drugs to suppress tissue rejection. They began with a 7 cm segment of trachea from a 51-year-old woman who had died of a brain haemorrhage. After stripping the trachea of all its potentially antigenic cells, the scientists reseeded the cartilage scaffold with cells from the recipient – a culture of epithelial cells from her own right bronchus for the inside of the graft and chondrocytes transformed from her own stem cells for the outside. They grew both types of cell in specially adapted cultures before being transferred to the graft over four days in a newly developed bioreactor. Many months after surgery, she remained in good health. In a further development, a nanocomposite polymer was produced at the Royal Free Hospital which then acted as a scaffold for the patient’s own bone marrow cells, which was then transplanted in Sweden.
Orthopaedics and trauma
An increasing understanding of how important it was to the very severely injured to be treated in a major trauma unit handling many such cases, led to reorganisation of the service. According to a National Audit Office report, the UK death rate was 20 per cent higher than in the USA. London established a metropolitan-wide trauma service based on four major trauma centres – The Royal London Hospital, (Whitechapel), King’s College Hospital, (Southwark), St George’s Hospital, (Tooting) and St Mary’s Hospital, (Paddington) – to which ambulances would preferentially take the comparatively small number of people with severe multiple injuries.
The conflicts in Iraq and Afghanistan had been accompanied by the development of new forms of weaponry, in particular improvised explosive devices. These led to severe injuries, often characterised by blast damage, flying debris, crush injuries and major burns. Blast injuries to the brain were common, and military surgery techniques developed rapidly to deal with these problems. The effectiveness of the medical care was such that 90 per cent of those seriously injured now lived, albeit often with horrendous injuries.
The earthquake near Port-au-Prince in Haiti in January 2010 showed how a disaster, if it decapitated a country by removing its centre of government, health service, police and transport facilities, could create vast difficulties for international relief effort. Organisations such as Médecins Sans Frontièrs (MSF) struggled to provide aid in a country with no functional port and minimal airport facilities, in the face of some 200,000 deaths and vast numbers of crush injuries. This was in contrast to the co-ordinated response in Japan to the earthquake, tsunami and nuclear power station problems of 2011. MSF was engaged at any one time in a dozen or more countries, sometimes being refused access for political reasons.
Assessments of a common procedure – arthroscopy of the knee – showed that there was little improvement for most people, and cast doubt on its efficacy.
Hip replacement
Hip replacement was perhaps the most successful orthopaedic operation ever, with 70,000 performed annually in the UK. A variety of operations included:
- Metal-on-Polyethylene: The ball is made of metal and the socket is made of plastic (polyethylene) or has a plastic lining
- Ceramic-on-Polyethylene: The ball is made of ceramic and the socket is made of plastic (polyethylene) or has a plastic lining
- Metal-on-Metal: The ball and socket are both made of metal
- Ceramic-on-Ceramic: The ball is made of ceramic and the socket has a ceramic lining
- Hip joint resurfacing.
The conventional metal on polyethylene hips do not last forever; wear means that revision is required, particularly in younger active patients. In search of a more durable option, metal-on-metal replacements, increasingly accurately machined, promised to end prosthesis failure. However, there was growing concern about them because the metal ball and the metal cup slide against each other and some tiny metal particles may wear off and enter into the space around the implant. Some of the metal ions from the implant might even get into the bloodstream. As a result, patients might develop pain, swelling and permanent disability. Revision operations were needed and problems became particularly apparent with the DePuy ASR, introduced in 2003 and withdrawn by the manufacturer in 2010 when some 93,000 had been produced. The process of approving and monitoring medical devices seemed in need of improvement.
Cardiovascular disease and cardiac surgery
Over the decades, the pattern of cardiovascular disease had changed dramatically. When the NHS began, patients clutched their hearts with angina or a heart attack and often died. Now thanks to drugs, surgery and imaging, they generally walked out of hospital. The drugs that had been developed proved useful in many forms of heart disease, spironolactone, ACE inhibitors, and diuretics. Many diseases; similar treatment. Now, however, there was far greater accent on breaking down apparently similar conditions into different diseases, as in the case of the multiple forms of cardiomyopathy. Each type had different genetics and, increasingly, a different form of treatment.
Statins, in use since 1987, are effective in preventing heart attacks in men with elevated cholesterol, and in members of both sexes who already have heart disease. They were increasingly prescribed to people at less and less risk of stroke or heart attack. Guidelines intended to save many lives by increasing the number receiving them were criticised by leading doctors, including the President of the RCP, because of their doubts about the underlying data and the ‘gross underestimation of of side effects,’ muscle pain and rarely myopathy and liver disease.
The collapse of Fabrice Muamba from ventricular fibrillation during a Spurs/Bolton match in March 2012 brought the issue of cardiopulmonary resuscitation dramatically to public notice. His survival, as a result of superb care on the pitch, in the ambulance and at a major cardiac centre was due to care from the first seconds following well developed protocols. It drew attention to the possibilities of bystander use of automatic external defibrillators (AEDs). In Denmark, cardiopulmonary resuscitation (CPR) was taught within the school syllabus, and AEDs were widely available in public places. Danish survival rates were the best in the world.
For some 20 years, percutaneous coronary intervention (PCI) – angioplasty with stent – had been available and increasingly used in the acute phase of a heart attack and for stable angina. In 2008, the Department of Health recommended that primary angioplasty should take over from thrombolytic drugs as the first-line treatment for myocardial infarction, as it was associated with lower mortality and better long-term outlook if carried out within three hours of onset. Second-generation drug coated (eluting) stents proved better than earlier ones. Ambulance services collaborated closely with their receiving hospitals and networks, the focus shifting from provision of early thrombolytic treatment outside hospital to identifying those patients with a heart attack who might benefit from primary angioplasty and rapid admission. Both coronary artery bypass grafting (CABG) and PCI could improve stable angina; neither significantly reduced survival or the risk of subsequent myocardial infarction.
The diagnosis of arrhythmias, for example, atrial fibrillation – a significant cause of embolism and stroke – was improved by the introduction of increasingly sophisticated recorders, some implantable. Novel anticoagulants, such as dabigatran and rivaroxaban the former was marketed as not requiring control, an advantage over warfarin. It proved to be just as associated with dangerous bleeding and that monitoring blood levels reduced this. The use of aspirin was discouraged by NICE. Surgical ablation was increasingly successful, although several procedures might be required to obtain 80 per cent or greater success rates.
Artificial hearts
Steady progress was made with total implantable artificial hearts. The Jarvic 7 (first used in 1982) was joined by the CardioWest™ Total Artificial Heart, developed in Tucson Arizona. By 2009 this had been used in over 800 patients. Often used to buy time in a seriously ill patient while a heart transplant match was found, it was used at the Cleveland Clinic early in 2009 for the world’s first Total Artificial Heart before a double heart and liver transplant. This operation was successful four times out of five, and the success of subsequent heart transplantation was one-year and five-year survival rates of 86 and 64 per cent.
Vascular surgery
Once a sub-specialty of general surgery, with a general surgeon undertaking vascular arterial procedures such as repair of abdominal aortic aneurysms, carotid stenosis and surgery on arteries in the leg, vascular surgery emerged as a specialty in its own right. Patients achieved the best outcomes following surgery at a hospital with a high volume of cases, by a vascular specialist team. In London, 75 per cent of surgery took place in six hospitals and 25 per cent was spread across another 12. To improve outcomes there was national pressure to concentrate services and reduce the number of centres.
Patients with significant narrowing of their carotid arteries are at increased risk of stroke. Those with transient symptoms have the highest risk of stroke in the period immediately following the onset of symptoms. The greatest benefit from carotid operation was seen if the procedure was carried out quickly following onset of symptoms. Both NICE and the National Stroke Strategy set targets for the time from symptoms to intervention, but access to immediate assessment and surgery varied widely, being worst in small volume units and best where services were linked to a large centre always able to provide urgent care, as in London where a few hyperacute stroke centres were created. In skilled hands, the risk of stroke and death from operation was no more than 3 per cent.
Ophthalmology
The introduction of new forms of imaging such as optical coherence tomography provided a new diagnostic tool that made it possible to examine the detailed structure of the retina and its response to treatment. The images were of high resolution, safe and quick to take, even in children. Initially the depth of the images was limited, but this was gradually overcome. Simpler equipment was introduced to test for glaucoma. Multifocal lenses were tried in the treatment of cataract, but did not prove wholly satisfactory. New drugs for the treatment of glaucoma were approved for general use by NICE and success was reported in the use of stem cells in the treatment of a rare form of inherited blindness, Leber’s congenital amaurosis. Age-related macular degeneration, earlier treated by laser, was now managed by biologics, anti-vascular endothelial growth factor drugs, Avastin and Lucentis, (administered into the vitreous), representing the new era of biological medicines for the management of neovascular disease. Anti VegF drugs could also be applied to retinal vein occlusion.
Cancer
Survival in the UK from cancer still lagged behind other European countries, with 250,000 diagnoses annually in England, and 130,000 deaths. Earlier diagnosis was an aim – a quarter of cases were first diagnosed in an emergency situation. Delay on referral, delay in hospital care in overstretched departments, inadequate capacity, the need to use many outdated machines, and paucity of state-of-the-art equipment such as intensity modulated radiotherapy, could be contributing to lower survival rates in England than in many European countries. A Vanguard Plan for cancer was developed to improve outcomes, that identified centres of excellence and linked hospitals treating cancer into networks.
Cancer vaccines
A new form of treatment for cancer was emerging, which involved the identification of the genetic makeup of an individual’s cancer, and developing a vaccine to destroy it. Many different approaches were under trial.
Radiotherapy
Radiotherapy techniques advanced, and proton beam therapy, using a high-energy beam of protons from a cyclotron rather than X-rays, became available at Clatterbridge Hospital, Wirral. Other units were planned for The Christie in Manchester (opened 2018) and University College London Hospitals (UCLH) in London (opening in 2020), as growing evidence supported its niche role to cure certain tumours without damaging vital organs. These centres would obviate the need for NHS patients to be sent abroad to one of a dozen centres in Europe and the USA.
Because of their relatively large mass, protons scatter less in the tissue; the beam does not broaden much and stays focused on the tumour shape without much damage to surrounding tissue. All protons of a given energy have a certain range; no proton penetrates beyond that distance. Although applicable to comparatively few patients, some, especially children, with highly specific types of cancer that occur in the retina, base of the skull and near the spine, may do better with this form of treatment than with conventional radiotherapy as it targets the tumour precisely, giving better dose distribution and not harming vital organs.
It was important to develop equipment that could target radiotherapy more accurately and precisely. Small tumours, inaccessible to surgery and near other vital structures such as the spinal cord, were then easier to treat. The gamma knife and CyberKnife delivered very narrow beams a few millimetres in width, so that several hundred beams could intersect on the tumour, instead of just a few. The CyberKnife had X-ray cameras that monitored the position of the tumour and sensors that monitored the patient’s breathing. This enabled the robot to reposition the radiotherapy beam during treatment to minimise damage to healthy tissue. It moved with the patient’s breathing and could track a moving tumour. Because of its accuracy, it allows larger fractions (doses) of radiotherapy to be delivered, so that the patient required fewer hospital visits. Visits for lung cancer patients could be reduced from 30 to three; for prostate cancer patients, visits could potentially be reduced from 37 to five and visits for palliative radiotherapy could be reduced from ten to one.
Photodynamic therapy
Photodynamic therapy was added to the classic treatments – radiotherapy, surgery and drugs – although far more limited in application. A photosensitising agent was injected into the bloodstream, absorbed by cells all over the body but stayed in cancer cells longer than in normal cells. Approximately 24 to 72 hours after injection, when most of the agent had left normal cells but remained in cancer cells, the tumour is exposed to laser light.
Chemotherapy for cancer
To the hundred or so drugs already in use for cancer, some 40 more were heading towards a licence, mostly effective and all expensive. Most derived from new knowledge of how cancer cells worked and it became essential to develop new tests of effectiveness. Advances in knowledge were often small but, in total, increased the chance of a favourable outcome. With increased length of survival came new complications, increased deaths from cardiovascular disease and sometimes infertility, problems most marked among teenage and young adult survivors.
Malignant melanoma of the skin was now the most common cancer in young women, increasing significantly over the previous ten years. The increase seemed associated with tanning and sun beds, and warnings of the health risks did not seem to be taken seriously by the young. The BMA had campaigned for controls on their use; a private member’s bill was introduced in 2010 to restrict their use by those under 18 years of age and was passed with cross-party support.
Bowel, cervical, breast and prostate screening programmes became responsibilities of Public Health England. Screening for bowel cancer by testing faeces for blood was introduced in the UK in 2007 and was steadily extended to cover men and women nationwide up to the age of 75 years. Computer simulation suggested that it might save 2,500 lives annually in the UK. However one-off five-minute screening by flexible sigmoidoscopy, (colonoscopy was already widely accepted on a five-yearly basis in the USA for those over 55 years), was shown in a prospective trial by workers at Imperial College to reduce mortality by 43 per cent compared with controls, as it offered the chance to remove polyps that might be pre-cancerous. For every 400 patients screened, one life would be saved.108
Mammographic screening was more contentious. There was increasing concern about the damage from unnecessary operations following screening, particularly as the public information leaflets seemed to underplay the risk. In both Canada and the USA, taskforce guidelines discouraged routine mammography before the age of 50, and suggested screening at wider intervals, every two to three years. The Independent UK Panel on Breast Cancer Screening led by Professor Sir Michael Marmot reviewed the evidence in 2012 finding that, for every 235 women invited for screening, one breast cancer death will be prevented and the benefits outweighed the harm done.109 His statistics were immediately challenged. False positives remained a problem.
Genetic Medicine
Medical genetics was coming of age and there was pressure for increased investment by the NHS. For 20 years, knowledge of the genetic causation of some diseases had increased, opening the path for the development of treatment and leading to therapies that altered the patient’s genetic structure. When a child had an unexplained congenital disorder, its genome could be compared with its parents to spot the difference. Genetic testing of a tumour could identify mutations that might be targeted by ‘smart’ drugs. The genome of bacteria could be ‘fingerprinted’ to trace and eliminate the source of outbreaks. In 2014 a network of regional diagnostic centres was established, with plans to assess the genetics of 100,000 cancer patients.
Substantial progress was made in the mapping of the genetics of lung cancer, which could be subdivided into many different types. Deeper understanding of the genetics of non-small cell lung cancer led to the development of small molecules to target genetic mutations known to play critical roles in the progression to metastatic disease, and the development of many new agents that inhibit the activities of specific molecules related to tumour growth, invasion, or metastasis. Women with a BRCA1 mutation have an 80 per cent chance of developing breast cancer and a 60 per cent chance of developing ovarian cancer during their lifetime. In 2009, the first baby was born in the UK as a result of pre-implantation genetic diagnosis and in-vitro fertilisation, as a result of which not only would she be likely to avoid these diseases, but she would not pass the increased risk on to her own children.
Effective treatment for rare disorders could come at high cost, as in the case of eculizumab, a humanised monoclonal antibody for atypical haemolytic uremic syndrome, an ultra-rare genetic disease that causes abnormal blood clots to form in small blood vessels throughout the body. The discovery in 1989 of a gene regulator in cystic fibrosis led, in 2012, to a regulator-based genetic treatment that showed promise in decreased cough and sputum production and which, if administered early, might reduce serious lung damage.
Human embryonic stem cells, first grown in 1998, could now be developed to the point of differentiation into different tissues in sufficient quantities for use in animal trials. In 2010, surgeons in Atlanta, in a hospital specialising in brain and spinal cord injury, injected a spinal cord injury patient with human embryonic stem cells in a federally approved trial to determine safety and, the following year, a trial of stem cells in multiple sclerosis began.
Gastroenterology
Flexible endoscopes and colonoscopes had made it possible to examine perhaps half of the gastro-intestinal tract, but the procedure was uncomfortable and usually required sedation. A new test became possible with the development of a PillCam that could be swallowed. It combined a camera that could take five to 30 photos a second, with LED lighting, batteries and a radio transmitter and was approved for use by NICE. Organ-specific PillCams were developed for the oesophagus (which could look forwards and backwards), the small bowel, and the colon. The device was particularly useful in diagnosing bleeding of obscure origin, and cancer of the colon in people who refused conventional colonoscopy.
Rheumatoid Arthritis
Until the 1990s, patients with this disease were treated with aspirin or non-steroidal anti-inflammatory drugs and modifying anti-rheumatic drugs such as methotrexate were only introduced when the disease had progressed. As a result, there was substantial permanent joint damage. Many new drugs now became available, most being ‘biologicals’, developed and produced in live cell systems. With better control and assessment, these drugs were now used much earlier to retard the progression of the disease, but had significant side effects.
Diabetes
Diabetes was emerging as an ever more important problem because of its link to obesity and the growing obesity in the population. Children were being diagnosed ever more frequently. Guidelines now promoted the use of the haemoglobin A1c as a faster, easier diagnostic test that could help reduce the number of undiagnosed patients, identify patients with prediabetes better and make control of diabetes easier. A1c measures average blood glucose levels for a period of up to three months. Diabetics could have this test every three months to determine whether their blood sugars have reached the target level of control that might minimise future complications. By the end of the decade, scanning devices were in widespread use to measure glucose in interstial fluid without taking blood. Transplantation of the pancreas or islet cells was now occasionally undertaken and could improve diabetic control.
Neurology
Hopes of better treatment for multiple sclerosis, a serious and disabling disease of the brain, were raised in 2008–10 by trials of monoclonal antibodies, such as Alemtuzumab, that target CD52 on lymphocytes and monocytes. Three large randomised trials of two new oral medications for relapsing-remitting multiple sclerosis showed that they reduced the risk of sustained accumulation of disability compared with a previous drug, but had dangerous side effects. Adverse effects were, in some cases serious, even lethal. Herpetic infections were seen and resulted in two deaths in the trials, and thrombocytopenic purpura developed in three patients.
Stroke
Because of its massive impact on people and the NHS, stroke services became a national priority; control of blood pressure, obesity and smoking were the key in prevention, but rapid recognition was essential to reduce long-term disability. Transient ischaemic attacks affected 40,000 people a year, and 10 per cent had a stroke within a week. Their assessment was often inadequate, if there was assessment at all. More stroke physicians were appointed and all hospitals created a stroke unit, though many did not offer an immediate scan, and not all patients were admitted to an appropriate unit.
Outcome was critically dependent on the speed of thrombolysis and, to achieve the rapid imaging necessary within half an hour of admission before thrombolysis was considered, reorganisation of services was needed. In London, eight hyper acute stroke units (HASUs) were established to which all patients were preferentially admitted. Diagnosis by ambulance personnel proved highly accurate and virtually every patient needing thrombolysis got it, some 17 per cent of admissions. Mortality from stroke fell 20–30 per cent. HASUs were supported by stroke recovery units, and transient ischaemic attack services for possible minor strokes. Outside the conurbations, this model was harder to apply. Centralising services in rural areas would be likely to increase ambulance travel times but NHS England believed that, where possible, 24/7 access should be introduced and services centralised.
A possible advance was interventional neuroradiology. The delivery of thrombolytic agents within four to five hours through a microcatheter directly into the thrombus, could help to restore the arterial supply and reduce mortality. Nationally, stroke mortality fell somewhat, but probably only one in three of those who would benefit from thrombolysis got it. Mechanical thrombectomy for those with ischaemic stroke, removing the clot with a stent, was shown to produce benefits if performed within six to eight hours, and was progressively introduced nationally in 2017.
Geriatrics
Acute wards in hospital were now largely populated by the elderly, as geriatric and acute services were now generally combined at least in the acute phase of illness. Yet the care of the elderly was frequently found wanting. Many forms of treatment were quite as effective in the elderly as in younger adults, but particular care was needed at the end of life. There was a major drive to ensure that all dying patients, and their relatives and carers, received a high standard of care in their last days. The Specialist Palliative Care Team at the Royal Liverpool University Hospitals and the local Marie Curie Hospice developed the ‘Liverpool Care Pathway for the Dying,’ (LCP) to transfer the hospice model of care into other care settings.
The LCP was recognised as a model of best practice and recommended in the NICE guidance in 2004 and its End of Life Care Strategy in 2008, which provided guidance on supportive and palliative care for patients with cancer. In theory, it prompted staff to consider the continued need for invasive procedures and whether current medicines really were helping. The LCP was criticised by some newspapers, particularly the Daily Mail. In a rising number of cases, junior doctors had decided to place a patient on the LCP, relatives were not informed and patients were denied the comfort of basic care and drinks, or were given powerful painkillers that they did not need. This led to an inquiry conducted by Baroness Neuberger.110 Plenty of evidence received by the review showed that, when the LCP was used properly, patients died a peaceful and dignified death. But the review panel was also convinced that implementation of the LCP was not infrequently associated with poor care. The guidance might have been right, but it had often become an excuse for poor nursing. LCP was phased out to be replaced by individual end-of-life plans for patients who were dying, LCP was removed from NICE guidance, and new guidelines were issued.
Alternative medicine
‘Organised scepticism’, the requirement that scientific claims be exposed to critical scrutiny before they are accepted, had never appealed greatly to proponents of alternative medicine. Some of them believed that scientific principles just could not be applied to forms of therapy that were intensely individual, though others were keen to accept the trappings of tradition, the white coat and the appellation ‘doctor’. Promotional materials were quick to refer to studies that, when examined, proved either to be poor in quality or to be selectively or inaccurately quoted. Occasionally people whose scientific claims were questioned turned to the law to attempt to silence critics, rather than engaging in scientific debate. Sometimes they succeeded, but not always. When chiropractors threatened to sue over an article, the editor of the New Zealand Medical Journal asked them to “provide evidence, not your legal muscle.” Similarly a US judge dismissed a device manufacturer’s law suit by saying that the dispute should take place in the pages of a journal, not in a Court.
In 2010, the House of Commons Science and Technology Committee reported that, as there was so little evidence for homeopathic treatment, the government should stop funding it on the NHS, and the funding of homeopathic hospitals – “hospitals that specialise in the administration of placebos” – should not continue.111 The Royal London Homeopathic Hospital changed its name to the Royal London Hospital for Integrated Medicine, as only a minority received homeopathic treatment.
Proponents of alternative medicine frequently argued for “more research” while being loath to accept results when they were forthcoming. An assessment of good trials for chondroitin and glucosamine in osteoarthritis showed that they did not reduce joint pain or have an impact on narrowing of joint space, though apparently having no ill effects. Yet these products were widely advertised, for example, on the back of buses, and widely sold. Sometimes they were prescribed on the NHS. Why?
Government consulted, in 2009, on proposals for statutory regulation of acupuncture, herbal medicine, traditional Chinese medicine and other traditional medicine systems, and the result was, in general, favourable to this, partly because of the potential harm that could result from these types of treatment. The Health and Care Professions Council, (previously the Health Professions Council) subsequently oversaw voluntary registers of health-related occupations in which practitioners were not obliged to be registered in order to practice, as well as being the regulator for arts therapists, biomedical scientists, chiropodists/podiatrists, clinical scientists, dieticians, hearing aid dispensers, occupational therapists, operating department practitioners, orthoptists, paramedics, physiotherapists, practitioner psychologists, prosthetists/orthotists, radiographers, social workers in England, and speech and language therapists.
Obstetrics and gynaecology
The pattern of maternity care was changing. Fifty years previously it had been the bed-rock of general practice – if one looked after a mother, one gained the family. Obstetric qualifications were valued in a new partner. However, over the years as the number of deliveries at home and in local units fell, GPs became less involved, less expert and – in medical school – less well trained. They became reluctant to be involved in care during labour, sensing their inadequate experience and being less available outside normal hours. Under the 2004 contract, GP maternity services were no longer paid for separately but as part of the global income, removing the incentive to involvement. Government and NICE policy documents now hardly mentioned GPs as participants in care. The King’s Fund reported that midwives were now the main health care providers for ‘low-risk’ pregnancies. Mothers could no longer turn to their doctor in the same way, and there was a risk of failure to ensure that relevant information was shared among GPs, midwives and hospitals. Pregnant women wanted continuity of care and post-natal support, which was in danger of being lost. NICE guidance in 2014 said that low-risk mothers might be booked in a midwife-led unit or for home delivery, including women pregnant for the first time, citing the greater probability of caesarian section, forceps delivery and episiotomy in a hospital unit. Patient satisfaction was higher for home birth and midwife-led units, though serious problems occurred in nine out of every 1,000 first deliveries at home.
The rise in the number of births strained maternity services. In 2012, there were 729,674 babies born in England and Wales, nearly half to mothers aged 30 or over. The number of births had increased each year since a dip in 2001 when there were 594,634 babies born. Increases in births were being driven by two main factors – increasing fertility rates among women born in the UK, many of whom had delayed child bearing, and the increasing population of non-UK born women of childbearing age. Probably because of the increasing number of pregnancies in older mothers, the number of cases of Down syndrome was increasing – from 1,075 diagnoses in 1990 to 1,843 by 2008 in England and Wales. Because of improved antenatal screening, more Down syndrome pregnancies were identified and more abortions took place. Teenage pregnancies, however, had been falling rapidly since 2008. About 180,000 abortions were performed annually in England and Wales, roughly 17 per thousand women aged 15–44 years. Virtually all were paid for by the NHS, roughly half being carried out under contract in the private sector. In some hospitals, it was the commonest day surgical procedure.
The Confidential Enquiry into Maternal and Child Health was continued as one of four Clinical Outcome Review Programmes (previously known as confidential enquiries) commissioned by the Healthcare Quality Improvement Partnership . The contract for the maternal and newborn programme from 2011, which includes perinatal mortality, was awarded to the National Perinatal Epidemiology Unit at the University of Oxford. The 2010–2012 figures showed a 10 per cent drop in mortality to 10.12/l00.000, mainly owing to a fall in complications of pregnancy. Three-quarters of deaths were, however, from coexisting medical problems, and these were not going down. An indication of maternity unit problems could now also be obtained from the results of litigation. Five thousand claims in the ten years between 2000 and 2010, a period covering 5.5 million births, involved cerebral palsy, and mismanagement in labour and mistakes in cardiotochograph interpretation. Human error, failure to recognise an abnormal reading or to spot damage was often to blame. More than half the cases of uterine rupture followed a previous caesarean section, and a report from the NHS Litigation Authority urged better consultant cover during labour.
In 2016, Julia Cumberlege chaired a review, Better Births, into maternity services in the wake of problems at a unit in Barrow. Her team argued for personalised care with choice of provider, a safer service with a standard investigation process when things went wrong, and a multi-professional approach with maternity hubs.
As the results of caesarean section improved, NICE controversially proposed that mothers be offered the choice of type of delivery and allowed to have a C-section as long as they were counselled about the risks. Antenatal care was reviewed, additional screening tests added, and complex systems introduced to monitor antenatal and care while in labour. However, technology was used, not just to improve health care, but to avoid legal claims. All babies had to be perfect, so caesarean section rates remained high. Recordings of babies’ hearts were kept indefinitely by some units as, in their absence, a future claim by parents of a handicapped child would be hard to defend. Babies had electronic tags, which made abduction difficult.
The treatment of urinary incontinence, often related to childbirth, was modified around 2000 by the introduction of vaginal tape and mesh. Within a few years, 10,000 or so operations a year were being performed. However, by 2016 it was realised that 10 per cent or more women had severe side effects from the operation and the procedure was rapidly discredited as first-line treatment. Its rapid adoption revealed weaknesses in the approval of devices for treatment, partly because long-term studies were inevitably impossible until general release. The involvement of manufacturers and the part played by financial involvement of doctors were components of the problem.
The demand for fertility treatment continued to rise. Older women were now eligible (up to 42 years of age) under NICE guidance, revised in 2013. In 2011 almost 50,000 women received treatment, average age 35 years, and some 13,000 babies were born. In the previous 20 years there had been roughly 200,000 births. The cost of a cycle of treatment was about £3,000.
A new problem emerged as a result of the practice of female genital mutilation in some cultures. Over a five-year period, nearly 4,000 cases had received hospital care in London, with the most at Guy’s and St Thomas’ where 1,146 victims were seen by staff.112 “These women have adhesions, vaginal infections, pelvic inflammatory infections, urine infections – for years they have been having these problems,” said a GP. Frequently a diagnosis was not made until the woman went into labour, when an emergency caesarean section might be required.
A further review of the long-term effects of hormone replacement therapy in 2017 showed no increase in all-cause mortality, or mortality from specific diseases, including cancer and cardiovascular disease.
Paediatrics
Neonatal intensive care
More babies needed specialist neonatal care because of increases in fertility rates for all age groups, particularly for women aged over 40 and under 20, the increased prevalence of assisted conception, and a 30 per cent increase in women admitted at 25 weeks of gestation or less whose babies need specialist care.
Over a decade the survival of babies born between 24 and 25 weeks improved as the details of care, monitoring and biochemistry were better understood. In the smallest babies, the outlook was unchanged; a fifth of babies born between 22 and 25 weeks had a severe disability, a figure unchanged since 1995. With each succeeding week, the results were better. At 26 weeks, babies stood an excellent chance of survival, particularly if they were delivered in, or rapidly transferred to, a large and experienced intensive neonatal care unit. Such units might have four or more neonatologists (spending more than half their time on the specialty and ventilating perhaps eight or more babies at a time). They had significantly better results than the smaller more numerous units. Transfer before delivery was best when a mother went into premature labour, but the capacity of labour wards sometimes made this difficult.
Neonatal screening
Screening of the newborn for metabolic disease had started in the 1960s with tests for PKU (phenylketonuria). Additions were made and the list expanded in England to include congenital hypothyroidism, cystic fibrosis, sickle cell disease, medium chain acyl CoA dehydrogenase deficiency and, in 2014, homocystinuria, maple syrup urine disease, glutaric aciduria type I and isovaleric acidaemia, serious but treatable disorders. In North America, the list of conditions for which screening was undertaken could be far larger, also including biotinidase deficiency, congenital adrenal hyperplasia and tyrosinemia. One private clinic would test for 20 different conditions, and genetic testing added to the possibilities.
Mental Illness
How many beds were needed? Between 1955 and 1995, the number of beds for mental illness and learning disability fell from 150,000 to fewer than 55,000. Over the next ten years, there was a further reduction of 30 per cent, care increasingly being delivered by community-based teams. While the number of admissions (perhaps for depression or dementia) fell, the number of those admitted ‘involuntarily’ increased by 20 per cent, particularly for drug and alcohol problems. Admissions for psychosis remained roughly constant. The case-mix of inpatient facilities was changing as the number of beds continued to fall, and increased use was made of private facilities providing specialist forms of care.113
Mental health policy had been based on the national service framework for mental health (1999), centrally agreed standards and a uniform model of care, home treatment, assertive outreach and early intervention teams. In 2009, the Secretary of State, Andy Burnham, published New Horizons – a shared vision for mental health, which grouped actions under a number of key themes: prevention, early intervention, tackling stigma, strengthening transitions, personalised care and innovation.114
In 2011 this was superseded by a Coalition document prepared in co-operation with many charities, No Health without Mental Health.115 Its goals were that more people should have good mental health and more who did not would recover; those with problems would have good physical health, would have a positive experience of care; fewer would suffer avoidable harm, stigma or discrimination. The following year, an implementation strategy was published with a commitment to improve access to psychological treatment as opposed to drug therapy, and to early intervention. The pressure on financial resources meant that the strategy did not include costly action plans.116
Southern Health Foundation Trust, one of the country’s largest mental health Trusts, was the subject of an adverse report in 2015 for failure to investigate properly over 1,000 unexpected deaths over the previous few years.
Learning disability
In the aftermath of care scandals at Winterbourne View, the government had promised to move patients out of such hospitals into the community. A report in 2014 showed that little progress was being made.
Dementia
The steady rise in the number of people with dementia, the costs incurred and the doubts about the effectiveness of treatment led to a national dementia strategy, Living well with Dementia, aiming for better knowledge, earlier diagnosis and improved care. Progress was being made in understanding the mechanism of Alzheimer’s but while there were drugs available and under development that modified symptoms, none as yet would halt the progression of the disease. Progress was made with tests that might indicate with a high degree of probability the later emergence of the condition, making it possible to identify patients at an earlier stage and possibly treat them.
General practice and primary care
General practice was in a mess. Roy Lilley blogged that there were not enough GPs nor enough in training, it was an increasingly pressured job, and fewer young doctors chose it as a career. Some GPs were taking home a shed-load of money, others were going broke, and practices where doctors were retiring might not be able to recruit newcomers. GPs were given the keys to commissioning but had not demonstrated superior abilities. They were accused of not keeping people out of hospital, told that they should make it easier to get them home faster, to open seven days a week without additional money, were rebuked for inadequacies over cancer diagnosis, the drugs bill and accused of overprescribing antibiotics. “GPs have caught in the neck.” From the early 1990s, through to the late 2000s, public satisfaction with general practice as measured by the British Social Attitudes Survey was more than 20 per cent higher than net satisfaction with the other parts of the NHS. Public satisfaction with general practice now had dropped by 7 percentage points in 2017 to 65 per cent, the lowest level since the survey began in 1983.
The problems were deep and systemic. The government responded and published General Practice: Forward View, a plan for the future in April 2016. Welcomed by the profession, it promised increased investment, a review of funding formulae, and the recruitment of more general practitioners. Shortly after the King’s Fund also published a report, Understanding the Pressures in General Practice drawing attention to the rising workload, the difficulty of attracting not only GPs but practice managers and staff, and the increasing complexity of work. Medical advances and developments in preventive health care had led to a considerable increase in the number of activities carried out in general practice. Telephone contacts, and contacts with nurses, increased substantially.
GP numbers and workload
Over the years the work of the GP had changed radically. With an accent on health promotion and the management of chronic diseases, payment systems were partly based on ensuring that patients were reviewed and targets met. As a result, a substantial effort went into reviewing patients, calling them in for review and, as the GP’s computer would flag this up when a patient came with something else, they would deal with multiple problems and fewer patients fell through gaps in the system. Care in areas of deprivation improved. Practice nurses increasingly took on the diabetes, asthma, chronic obstructive pulmonary disease and blood tests. GPs inevitably spent more time on administrative and financial matters and, in many areas, local practices linked for organisational and educational reasons.
The Department ceased to commission activity data in 2008. The Nuffield Trust drew what was available together in its report Is General Practice in Crisis? (2014). The number of general practitioners was rising steadily if slowly, though not fast enough. Between 1997 and 2007, the increase had been 19 per cent, from 28,046 to 33,364. From 2006– 2013, the rise was 4per cent and, in terms of population, there was no expansion. They might be poorly distributed. In the majority of CCGs, there were 35–45 whole-time equivalents for 100,000 patients, but there were outliers, for example, far fewer GPs in Slough than in Devon, a situation that the old Medical Practices Committee would never have tolerated. A GP workforce crisis was emerging. Not enough GPs were being trained, more worked part-time, and more existing GPs planned to retire early. A cap on the size a ‘pension fund’ was a factor; when this was reached, some doctors thought the tax implications of continuing to work in a stressful job made it not worthwhile. The percentage of women rose from 31per cent to 42 per cent. Men worked more sessions and more women were part timers.117 While most GPs were partners in their practice, a growing proportion were salaried, by 2015 almost a third. They were employed by other GPs or commercial companies who tendered to run practices. Three-quarters of partners worked full time (44 hours/week), less than half of the others did so, and an increasing number of entrants wanted to work part time. On average, practice staff worked a little over half time. GP consultations averaged 11 minutes – substantially longer than 16 years previously, and nurse consultations lasted a quarter of an hour. One GP in ten was involved in commissioning services, far more were acting as the lead within their practices.118 General practice, though ahead in IT, lagged far behind the hospital service in developing systems of clinical governance, measuring activity and systems that followed up patients with identified health care needs did so priarily for financial reasons. Consultants questioned how far it was safe to transfer significant care to the community, if patients were all too easily going to be lost to the system.
Access to the practice
Easy access to ‘the doctor’ had long been a problem. In 1948, patients turned up and waited – and, in some places, patients still do. In the 1960s, appointment systems were introduced. The NHS Plan set a target that one should be able to see a health professional within 24 hours and a GP within 48 hours. Incentives were introduced, PCTs supported practices, the Prime Minister launched a Challenge Fund, and the National Primary Care Development Team promoted a scheme based on American ideas of quality improvement (but where waits could be very long indeed.) A new approach, “Advanced Access,” suggested that appointments were made on the same day, rather when people wished. Originally hailed with hyperbole as ‘the answer’, it too led to frustration because, as appointment slots were held for ‘urgent problems’, the delay for a routine consultation got longer and surgery phone lines were blocked early each morning as patients fought to get through. Other strategies employed were telephone triage, telephone consultations and delegation to minor illness nurses or HCAs. These techniques had little effect on patient access, or the satisfaction of staff or patients as improved access increased demand.
Julian Tudor Hart viewed the changes with concern.
Bit by bit, community generalist doctors are sliding away from all those roles that connected the NHS with the real world of raw, unsorted complaint. For many GPs that will be a relief. For anyone interested in developing community generalists as imaginative resident human biologists, with continuing responsibility for the health of defined populations, it’s a cause for extreme concern.119
He felt that the gatekeeper function of the GP was important and was being undermined. GPs meanwhile often welcomed a role within hospital teams, and the transfer of tasks to nurses.
The politics of the profession were also changing. The RCGP was increasingly active in pushing a political as well as an academic agenda, and though an adviser to the Department of Health, Clare Gerada, Chair from 2010–2013, opposed many government proposals. She and her successor pushed political campaigns, for example, a higher proportion of the NHS budget on general practice. The College aimed to work with the BMA’s General Practice Committee, and the BMA appeared content to work together. After the 2015 election, government committed itself to increasing the number of GPs and their resources.
Changing the system
Regularly it was stated that general practice had to change; in 2013 NHS England published Improving General Practice – a Call to Action.120 Just what that action should be, or what changes were envisaged, was less clear. Sometimes it seemed about continuing the 50-year trend for doctors to work in larger groups, networks or federations. Generally it was a call for more resources for general practice, as in the College’s blueprint in 2015 under the new Conservative administration.
In 2007, the RCGP had published a ‘Road Map’, the key idea being that doctors and their practices might come together in ‘federations’ to deliver better services in a more co-operative way.121 Federations might strengthen the capacity to develop new services out of hospital, tender for services, make efficiency savings/economies of scale, (for example, in back office functions), improve local service integration across practices and other providers, strengthen clinical governance, improve the quality and safety of services, and develop training and education capacity. This vision for the future was updated in 2013 in an aspirational document, The 2022 GP, A Vision for General Practice in the future NHS.122 Acute Hospital Trust medical directors saw the advantages of working with local general practitioners, who were now often central to commissioning decisions. Many practices began to develop organisations and networks to try to improve care, commission or provide services or both. The Nuffield Trust, the King’s Fund and Hempsons (solicitors), published a toolkit to assist practices to develop new structures and learn from others’ experience.123 Throughout the country, some GPs were trail-blazers in coming together on a geographical basis. Often the motive was to create an organisation that could bid successfully for contracts – and thereby prevent other groups or private sector organisations from moving in. Sometimes it was to help to achieve a better quality of service.124 The Department of Health selected 14 projects that straddled health and social care and aimed to offer patients, particularly those with chronic conditions, a single point of contact, whatever service they were seeking.125 The Newcastle-upon-Tyne NHS Foundation Trust published an ambitious manifesto on its website, Better Together, in 2010 believing that it was best placed to oversee integration. It set out to produce integrated clinical pathways involving hospital, community nursing services and primary care.126 KPMG, The Nuffield Trust and conferences considering primary care supported the federation of practices. In some areas, 100 or more were bonding together into large-scale providers, enabling their patients to access a variety of enhanced facilities and services. The Lancet said radical restructuring was needed to manage increasing patient demand amid cuts in resources. New models, more nurses, more doctors, half hour appointments, a salaried service and doctor-led telephone triage might all help. Simon Stevens of NHS England told the RCGP 2014 Conference that differing models might be needed, hospital Trusts providing GP services where practices struggled to recruit doctors, practice federations, or federations which expanded to include hospital specialists, community teams and social care.127 And, progressively, a variety of models emerged, the common factor being a local desire of GPs to associate for academic or business reasons, sometimes centralising services, sometimes reducing back-office overheads, to develop closer relationships with acute hospital Trusts, or to become a commercial enterprise.
Polyclinics and community services
Labour had pressed for increased community-based services. Both the programme for Transforming Community Services (2009)128 and the drive for polyclinics had their genesis in the Darzi reports. While never tightly defined, polyclinics would aim to combine general practice and some elements of hospital care with a range of health and support services, for example, benefits support and housing advice. General practices, a walk-in clinic, investigations such as breast cancer screening, and consultant sessions in, for example, cardiology and ophthalmology, might be co-located. Services such as X-rays and blood tests could be available. They might be open from 8am to 8pm every day, including at weekends, and available to people even if they were not registered there.
The financial crisis and a change of administration slowed projects. Those units identified as polyclinics differed because of local needs, priorities and physical and organisational legacies. No two were alike and there was difficulty reconciling local realities and the policy expectations being imposed. Some, such as Barkantine, were developed around existing systems. Others were new, for example, Heart of Hounslow, and the Loxford Clinic in Redbridge, opened in 2009, providing the premises for a practice, consulting rooms for specialties such as dermatology and ophthalmology, modest imaging facilities – but no parking. Few examples achieved the goal of community nursing and social service integration. Was Loxford – with a capital cost of £6.5 million and £2.5 million on equipment – an effective use of resources? It was an expensive policy and a planned evaluation of polyclinics was stillborn as the polyclinic policy was abandoned. The initial announcement in 2008 of the first seven in London proved a flash in the pan. Five years later a practice and some extended services might still exist, but these were little more than the vestigial remains of the initiative. A substantial number had closed down.
GP-led health centres
Experiments were tried in parallel. Another initiative to increase competition was GP-led health centres. In 2007 government required every PCT to tender for one, open from 8am to 8pm, providing walk-in services for unregistered patients and also registering them. The first such centre opened in Bradford in 2008 and, within two years, 12 had opened and 80 or more were planned. In areas where they opened, local practices were in competition and were soon extending their hours, for example, to Saturday mornings and into the evening. Many tenders were won by local GPs who formed their own companies or co-operatives. Others went to commercial organisations, often in partnership with GPs. The Chairman of the BMA’s Council, though opposing private sector initiatives, himself belonged to one of four practices that jointly bid successfully for a GP-led health centre in Bridlington. Some of the centres were imposed on PCTs where they were not required. Some, labelled as unnecessary and costly duplication of existing services, were closed. Others, though fulfilling a genuine need, seemed to have no effect on reducing hospital attendance. Similarly, walk-in centres did not have proven advantages.
Contracts
Partnership remained the gold standard, in the view of the BMA. Most money was determined by patient numbers, but the Quality Outcomes Framework (QOF) provided a significant addition, was simplified, and demonstrably affected practice performance. However, over 10–20 years, the number of salaried doctors steadily increased as did the number of ‘fixed-share’ partners, a system not unlike a salary. Salaried practice often suited young doctors, and large and business-like partnerships might take advantage of the situation. Salaried doctors had less commitment to the practice and earned less, perhaps £70,000 against £100,000 annually before tax. Before they were abolished, PCTs had an increasing influence on practices. A practice might find the PCT willing to fund new staff members in the practice team, for example, a physiotherapist providing open access to patients, or a psychotherapist. The PCT could bring pressure on practices to extend their hours of opening as well as use the quality and outcomes framework as an incentive.
Because of the massive and unanticipated increase in pay, in 2008 the Public Accounts Committee delivered a damning report on the 2003/04 contractual negotiations. Pay had risen an eye-watering 58 per cent because targets had been set too low.129 Subsequently, pay rose less than inflation and seniority payments made to GPs with long experience began to be phased out (at no financial loss to the profession as a whole). Gordon Brown, when Prime Minister, made extended surgery opening a priority. After acrimonious negotiation, general practices accepted changes to the contract for 2008/09, which would give GPs financial incentives to provide longer opening hours.
The Personal Medical Services contract (PMS) paid significantly more than the standard General Medical Services (GMS) contract – some £10 per patient. There was no correlation with these contracts and deprivation. In 2014, NHS England announced that this contract would be reviewed.
The Alternative Provider Medical Services (APMS) contract allowed PCTs to contract services from groups outside the NHS, including commercial and voluntary organisations. PCTs were slow to do so, mainly using the system to fill specific requirements, but by 2008 some 100 practices were being run by alternative providers and it was GP-led companies that had been most successful in bidding for these contracts. Corporate providers and social enterprises had been successful in a minority of cases. GPs had an in-built advantage in that, while they might be strangers to the complex process of tendering, they had local knowledge and the financial advantage of remaining within the NHS pension scheme. Some supported this initiative as encouraging innovation; others saw it as an aggressive commercial take-over of general practice.
Out-of-hours
Out-of-hours care was now patchy. The removal of the traditional 24-hour contract in 2004, a personal service no longer deliverable with the current workforce, was bad for patients. Few GPs wished to do much out-of-hours work, and there was an increasing trend among GPs to part-time working, reducing continuity of care even within working hours. The service, now managed by PCTs and later CCTs, was provided by a variety of independent organisations linked neither to hospitals nor to general practice, was flawed. The Times described the out-of-hours service as a disaster and an avoidable one, as a result of the way the Department of Health had allowed out-of-hours care to move from GPs to PCTs at minimal cost to the doctors.130 GPs had given up £6,000 and the new service cost £13,000 per doctor. Sometimes federations of general practices provided out-of-hours cover. Increasingly a hub model, in which out-of-hours primary care, a hospital A&E and other services were contiguous, emerged.
The Healthcare Commission, reporting on emergency and urgent services in September 2008, found gaps and variation in performance.131 Not all services met the standards for prompt assessment. Running the out-of-hours services was hard; some organisations went out of business suddenly. It was difficult to recruit local doctors, and medical liability insurance costing tens of thousands of pounds put them off. Services might look far and wide for staff, even to Europe. Often only a minority of those asking for a visit got one; “telephone diagnosis” was common. The population covered by an out-of-hours deputy might vary from 30,000 in some areas to 300,000 in others, and PCT spending on services varied widely.
NHS Direct, and later NHS 111, provided phone access and signposting, reliant on an algorithm-based computer decision system. Hospitals realised that someone experienced was needed at the front door; those staffing out-of-hours phones were generally junior. Such a system had to be risk averse. Few had the immediate back-up of an experienced clinician and often the only reliable service available 24/7 was the hospital A&E. There was a reliance on triage. Studies suggested that the decisions taken by ‘triagists’ varied and that a substantial proportion of them were wrong. Outcome studies did not reveal many problems as a result, possibly because most calls were only about trivial matters. The advice was given after too few questions and without properly interpreting the answers. The protocols used were hard to assess because they were neither publicised nor available online allowing them to be studied.
Administrations of all parties tried with some success to persuade GPs to keep surgeries open longer. The Prime Minister’s Challenge Fund offered pilot practices money to facilitate 24-hour telephone access and weekend surgeries as part of a major move towards radically extending GP opening hours, although there was not always patient demand. Following the 2015 election, government pressure for extended hours increased.
Quality in primary care
The QOF, introduced in 2004 and accounting for some 15 per cent of primary care costs and a significant part of a practice’s income, was modestly successful in improving processes of care as far as the conditions covered by the framework were concerned, though other aspects such as personal and continuity of care might be sacrificed in the process. It did not affect standardised all cause mortality. A system of financial incentives, it covered clinical care, organisation, patient experience and additional services. Incentives are often successful and QOF led to consistent improvements for intermediate outcomes such as blood pressure and cholesterol, and secondary prevention was promoted. Long-term disorders were identified and treated in the practices, often under nursing supervision. Significantly, practices in deprived areas achieved similar levels of cover to practices in more affluent areas, and QOF appeared to be a way of reducing inequalities of care. The framework was altered regularly, seven times by 2010. It was supervised by primary care academics, overseen by the RCGP and lay representatives and incorporated advice from NICE. The challenge was discarding less-effective components, introducing new ideas and considering value for money. It increasingly took account of disease prevention and outcomes but its increasing complexity led to a decision to reduce its scope and the money that was attached to QOF.
The King’s Fund commissioned an independent inquiry into Improving the Quality of Care in General Practice. The report said that, while standards and quality were generally good, there was room for improvement and its report was an important reference source.132 Variations, sometimes unacceptable, were found in quality of diagnosis (for example, cancer) and prescribing. Referral rates also varied, with little relationship to patient outcomes. Patients might be unable to see their preferred doctor rapidly, preferring to wait for him or her, and continuity of care and its co-ordination might be lacking. There was a lack of data and of transparency about what was being done. Doctors needed to adapt more to the changing world, technology and patients’ expectations. Without much supporting evidence, the inquiry thought that a move from isolated practices to federated networks was required and radical change was needed, a new deal for patients, and a change from the practice as a gatekeeper to a navigator within the NHS. The inquiry wished to find new measures of quality in primary care, “a task we were unable to complete.”133
In 2013 the CQC began its programme of surgery inspection starting with a list of practices already considered by PCTs/CCGs to be among the worst. Not surprisingly, a significant number fell short, sometimes because of hygiene and cleanliness, sometimes because of staffing problems. CQC uncovered a catalogue of failings at more than 300 practices; far more passed muster but the horror stories included maggots on the floor of consulting rooms, patients given out-of-date medicines or injections, and nurses not trained in basic first aid.134
Health service information systems
The Internet was now a major source of health information to patients, and few patients faced with a serious illness failed to Google it. Could Twitter and social networks help to identify disease outbreaks? Twitter certainly drew attention to major commercial problems and sometimes led to urgent action to solve them. Could it also reveal NHS scandals? NHS Choices provided information and assistance on choosing health care providers, a self-help guide which might lead one to consult a doctor, and a health encyclopaedia. Many thousands of apps on smart phones were introduced, from those designed to improve general ‘wellness’ to others that monitored medical conditions. Some were helpful, for example – one to calculate how much fluid a badly burned patient needed – and were, in effect, medical devices. Most doctors used them. For the majority, there was no evidence that they did any good.
The NHS IT programme continued to miss targets and produce problems and featured in reports from the Audit Commission and the Public Accounts Committee.135 The promise of a paperless NHS by 2006 now appeared fatuous. Deadlines were missed, technologies might be more cumbersome and time-consuming, and sometimes less safe. Hospital Trusts were now permitted to install their own system if compatible with the national network. Suppliers and the government were locked in contractual disputes and the philosophy and ambitions of the programme were questioned. In 2009 the first Summary Care Records (a secure electronic summary of key health information derived initially from the patient’s GP record) began to be rolled out but the ‘patients’ portal’ had been abandoned. In 2010 the programme was scaled back. Money would be saved by abandoning uniform software if hospitals already had a system fit for purpose. The successes, NHSmail, PACS and Choose and Book, were overshadowed by the now admitted failure of the core innovation, a standard centrally procured electronic records system across secondary care. However, few other countries had been more successful in the introduction of a national system. In October 2010 the Department consulted on new proposals – Liberating the NHS: an Information Revolution.136 Progress remained slow and, in 2011, the Audit Commission doubted if the centralised top-down system could ever be made to work at justifiable cost. In August 2011, the Public Accounts Committee examined the delivery of care records systems under the National Programme for IT and said that the central spine and e-record for all patients was unworkable, that major parts of the NHS were already using local and effective systems of intercommunication not compatible with other systems, and ambitions should be curtailed to prevent waste of money.137 The cost, up to March 2011, had been £2.7 billion. The Cabinet Office’s Major Projects Authority said that the National Programme for IT had not and could not deliver its original intent. The dismantling of the programme was accelerated and replaced by cheaper regional systems, the Board managing it was abolished, and control returned to the Department while a further IT strategy was developed. Published in May 2012, The Power of Information was long on vision and short on specifics, deadlines and costs; at its heart was how information should be shared. Patient data should be shared by all health and social care professionals that needed it. Patients should have access to their data, and anonymous data should be used by the NHS, researchers and industry to promote quality and innovation.138 In the real world, financial break-even seemed decades away.
A key component, Care.Data, approached completion, although it was delayed by public uncertainty about data security. It aimed to aggregate health information from a variety of sources – hospitals, GPs, community services and prescribing – linked by NHS number and postcode. Linkage would provide a basis for research and ultimately might assist the personalisation of treatment to assist the best patient outcome. It was abandoned in 2016, dogged by lack of trust in its confidentiality.
A new emergency phone number, NHS 111, was introduced to replace NHS Direct to improve access to non-emergency services, first in the north east in 2010, and country-wide in 2013. It was not for life-threatening problems, but for when help was nevertheless needed fast. The clinical content was controlled by a national clinical reference group chaired by the RCGP. The introduction was a near disaster. Before it went live, the BMA warned that the system was inadequate and would produce problems. There were reports of dropped calls, long waits and poor advice. NHS Direct had been staffed by nurses, while 111 used lay operators following a computer protocol. Inevitably they played safe. NHS Direct had advised half the callers that they could care for themselves. This fell to 15 per cent with NHS 111. As a result, referrals to hospital A&E departments and GPs rose substantially, straining the systems. “A disappointing start”, commented a Minister. However, it was steadily developed; general practice out of hours and NHS 111 were steadily combined, and it was planned to move some callers to websites and apps, increasingly oriented (like ‘Babylon’) to diagnosis and treatment recommendations.
Dr Foster launched its own hospital and consultant guide that had far more specific information on hospitals and individual consultants. Wikipedia, was used by so many people to explore the options for treating cancer, that it became important to maintain its accuracy and Cancer Research UK undertook to edit and update articles. Even nineteenth century archive material, such as the BMJ and The Lancet, was now available online and at PubMed.
Hospital and specialist services
Between 1987/88 and 2016/17, the total number of NHS hospital beds fell by approximately 52.4 per cent – from 299,364 to 142,568. Innovations such as day case surgery and better rehabilitation of patients helped the NHS cope with fewer beds, but had changed the nature of hospital care substantially. The RCP warned against any further reduction, given the intense and growing pressure which occasionally forced major hospitals to close their doors to ambulances and emergency admissions.
Average number of beds available by category, England, 1987/88–2016/17
Day only
Learning disability
Maternity
Mental illness
General and acute
Source: NHS England 2017 and King’s Fund briefing on hospital beds, September 2017
Independent sector treatment centres were failing to provide good value; though paid above tariff levels, few delivered more than 90 per cent of the services for which they were paid during the first five years of the contracts. Waiting list work from NHS units was sometimes transferred, but it seemed unlikely that all independent sector treatment centres (ISTCs) would justify renewal of contracts or succeed when payments moved to tariff levels.
Accident and Emergency (A&E) departments
The pressure on A&E units rose steadily. Targets that required departments to treat, admit or discharge 98 per cent of patients within four hours had improved the A&E experience for patients, while changes that allowed GPs to opt out of providing out-of-hours services had probably increased A&E use. The move from NHS Direct, which had overcome its own teething problems, to a new emergency enquiry phone number (NHS 111) proved initially calamitous, so it was logical for people to seek out the red and white signs for A&E, indicating some of the best triage nurses, consultants and registrars in the world. Many planned their attendance well ahead and, because of past experience, did not try other ways of getting attention. Increasingly minor illness units, co-located with A&E, helped by seeing a third of those attending, but the rise in visits was a testament to the success of A&E units and the failure of an important part of primary health care.139 That there were nowhere near enough A&E consultants added to pressure to close units that had poor cover. Sir Bruce Keogh, Medical Director of NHS England, reviewed urgent and emergency services.140 He suggested improvements to urgent services outside hospitals, to the telephone 111 service, the greater use of paramedics to screen urgent calls, and a division of hospital A&E departments into the majority that could assess and start treatment for all patients arriving, but which would transfer the small number of patients needing specialist treatment to more comprehensive “major emergency centres.” His was a three- to five-year plan with no costing or suggestions as to how it might be accomplished in the face of local pressures. It was a road map rather than an urgent solution to problems. The Daily Mail ran a campaign showing death rates of emergencies had increased following the closure of A&E in Newark, Notts.141 Pressures continued to rise.
Hospital building
The NHS Plan (2000) had announced a major building programme, largely funded by PFI, to modernise the ageing NHS estate, half of which dated from before 1948. As a result, capital stock was now better. It was down to 20 per cent pre-NHS with 100 schemes completed and many others under way at a cost of £12 billion. Department of Health guidance suggested that new hospital wards should contain at least 50 per cent of accommodation in single rooms. Maidstone and Tunbridge Wells Trust replaced its ageing Pembury Hospital with the NHS’s first all-single room acute hospital, a £230 million PFI scheme in 2011. The new hospital provided all patients – except those in the special care baby unit – with their own en suite room. This was welcomed by patients’ organisations and anticipated that it might help to reduce cross-infection rates. Similarly, the new PFI development at the Royal London Hospital provided many single rooms.
Private Finance Initiative (PFI)
PFI was now seen as a problem, not a solution. The economic crisis increased the difficulties of Trusts with PFI schemes. In 2009 the Treasury announced plans to lend to recession-hit PFI schemes. A £1.5 billion bailout fund was established. Even the independent treatment centres were affected. The buildings and facilities of some 15 were purchased by the NHS.
Of 22 hospital schemes planned in England in 2007, two years later only 11 were being pursued. This was because of the credit crunch and the realisation that PFI locked hospitals into decades of fixed overheads, just when policy was to encourage a shift to care outside the hospital. In some cases up to 15 per cent of Trust revenue was predicated in this way. It was now accepted that PFI schemes were far more expensive than paying from public funds and, in November 2011, an in-depth review of PFI was announced, so that any future contracts were less of a drain on funds. The Secretary of State thought the financial stability of many Trusts was threatened by PFI but said hospitals would not be closed for reasons of debt. Trusts with major debts from PFI included:
|
Trust |
Debt (£ million) |
|
St Helens and Knowsley |
338 |
|
Oxford Radcliffe |
298 |
|
Buckinghamshire Healthcare |
92 |
|
Mid Essex Hospital |
163 |
|
South London Healthcare |
214 |
|
Barts and the London |
1,149 |
|
West Middlesex University Hospital |
60 |
|
Maidstone and Tunbridge Wells |
228 |
|
University Hospitals Coventry and Warwickshire |
379 |
|
University Hospitals of North Staffordshire |
274 |
|
Mid Yorkshire Hospitals |
311 |
|
Sandwell and West Birmingham |
377 |
|
Royal National Orthopaedic Hospital |
61 |
|
Wye Valley (Hereford) |
64 |
|
Dartford and Gravesham |
94 |
|
Walsall Hospitals |
170 |
|
Barking, Havering and Redbridge |
238 |
|
North Cumbria University Hospitals |
67 |
|
North Middlesex |
144 |
|
Worcester Acute Hospitals |
87 |
|
Portsmouth Hospitals |
236 |
|
North Bristol |
430 |
|
TOTAL |
5,474 |
Organisational change, hospital policy and reconfiguration
Changes to the hospital system continued to be urged as essential to the survival of the NHS and balancing the books, in spite of the length of time taken by such initiatives, their expense and frequent failure to progress and deliver the expected benefits.142 Sometimes inpatient services were transferred from a small hospital, for example, the 100-bed Queen Elizabeth Hospital II in Welwyn Garden City (the first post-war hospital in England), to a much larger and more modern one, for example, the Lister in Stevenage. The older unit might be re-equipped to provide an urgent treatment centre, outpatient facilities and diagnostic services. More substantial closures – for example, of accident departments – were unpopular, but the status quo might not be in patients’ interests. Political rhetoric stated that public opinion should be a key factor in reconfiguration, and many people and most MPs felt the proximity of a service was more important than its clinical outcomes. Conflict was inevitable.
Change continued, albeit slowly. The Central Manchester University hospitals absorbed those in Trafford that had a substantial deficit and clinical departments too small for effectiveness. The Academic Health Science Centres could also be so huge that major reconfiguration could take place within their organisation.
Darzi (2008) had maintained that the district general hospital pattern of the 1960s was no longer relevant because of the development of community services (for example, polyclinics) and the need for treatment, such as for heart attacks and strokes to be centralised.143 His chosen pattern was:
A local hospital, serving a population of around 250,000 would include a 24-hour A&E department, paediatric assessment unit, maternity unit, and provide inpatient emergency care alongside critical care services. In addition to other clinical services, it could also include a 24/7 polyclinic at its front door, treating non-urgent cases and providing direct access to diagnostics, tests and outpatients. This will prevent many unnecessary trips to A&E departments. There is not a one-size-fits-all local hospital as the range of clinical services must be driven by local need.
Urgent or more routine illnesses might involve community services, a polyclinic, a local hospital or a major one. Financial models indicated how the income of hospitals might change as the pattern of work altered. He thought polyclinics were central to a reduction of the demand for, and the cost of, hospital services – particularly in London. The London School of Hygiene & Tropical Medicine was commissioned to undertake a two-year evaluation of the early polyclinics, but with a change in administration, the polyclinic policy was largely forgotten (as was the evaluation).
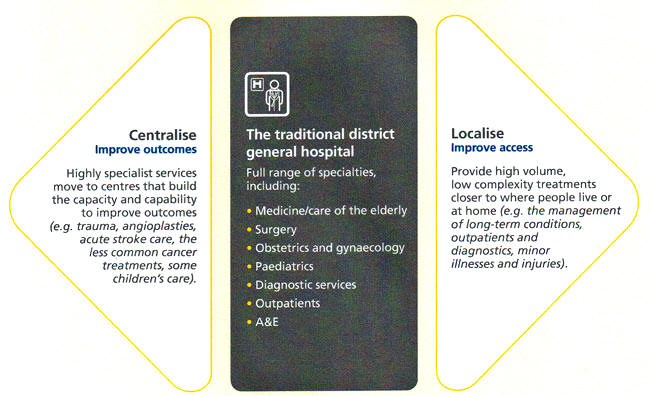
Source: A local hospital model for London. Health Care for London. 2008.
SHAs in general showed no enthusiasm for total reorganisation of their services. In most regions there were local issues to be resolved, and these were time-consuming enough. Darzi’s reports led the ten strategic health authorities to publish the results of their modest planning. London had been the most enthusiastic. The SHA-hosted Healthcare for London involving PCTs in the development of proposals. This examined types of care where outcomes could be improved by reorganising provision. Healthcare for London published substantive proposals in November 2008, for example, on a stroke strategy.144 In February 2009 it consulted on the case for four trauma units and ten hyperacute stroke units and, in July, the PCTs agreed major service changes. London’s trauma system, went live in April 2010, the 3–5 per cent of 999 patients critically injured being taken directly to one of four major trauma centres. The predominant types of major trauma were caused by: road traffic collisions; followed by stabbing injuries; and falls from a height.
Clinical outcomes might be improved by reconfiguration, as in heart disease, trauma and stroke (see below). Fourteen senior doctors, including College Presidents wrote to The Guardian in April 2010.
There has been a wealth of clinical evidence for many years that specialist clinical services, such as stroke, trauma and heart surgery, should be concentrated in fewer centres. This would allow the latest equipment to be sited with a critical mass of expert clinicians who regularly manage these challenging clinical problems, and are backed by the most up-to-date research. The greater volumes of patients mean doctors are better at spotting problems and treating them quickly. Survival and recovery rates would improve markedly with many lives saved. As techniques and technology have developed over recent years, speciality rather than proximity has become the key for patient safety. So increased patient safety and improved care must be the major drivers of any reconfiguration.
In London, reconfiguration of stroke services followed and cardiac services had already been changed, so patients went immediately to hospitals with 24-hour cardiac surgical facilities. In the north east of England, services had also been rearranged and other regions moved to follow this example by concentrating services into a smaller number of specialist units, establishing networks of services for hyper-acute stroke care, major trauma and vascular surgery where they could.
Paediatric cardiac surgery was examined after the problems in Bristol. In the 1970s when Guy’s started heart surgery on children, the Department of Health doubted whether London needed a third unit in addition to the Brompton and Great Ormond Street. Nevertheless, the unit was established and its results were good. A series of expert reviews over ten years had recommended that the 11 units carrying out children’s heart surgery should be reduced in number. A review was launched in 2008 by Sir Bruce Keogh, the NHS Medical Director. Some 3,000 operations a year were carried out, some in rather small units. The evidence was that outcomes were better in larger and more active units. In a report published in February 2011, it was suggested that four should restrict themselves to paediatric cardiology, not surgery – Oxford, Leicester, Leeds and the Brompton, the last being a large and excellent unit. The proposals were strenuously resisted and showed the difficulties of changing systems, not least because information on safety and workload was not always cut and dried.
An unusual option for service reconfiguration was the approach adopted by Moorfields Foundation Trust, so that, by 2013, people could attend a Moorfields unit in Bedford or at one of 17 other hospitals linked to the City Road site. The units were managed and staffed by Moorfields in a partnership with the local hospital. Hospitals would approach Moorfields for assistance in maintaining viable ophthalmic services, both sides benefiting.
Clinical networks developed as in cancer care. Hospitals of different types collaborated, so that patients requiring the most specialised care were centralised, while other hospitals provided the necessary local support and backup. Such clinical networks often developed at a professional level rather than by central diktat.
Reconfiguration under the Coalition and the Conservative administration
Following the change of administration in 2011, Andrew Lansley, no fan of strategic planning, slowed down the process of reconfiguration, making it harder to rationalise services and save money. Four key tests now had to be met: support from GP commissioners; public and patient engagement, including local authorities; greater clarity about the clinical evidence base underpinning proposals; and taking into account the need to develop and support patient choice. This decision led to the resignation of the London SHA chairman and some of the non-executive directors who were committed to proposals now at an advanced stage. There was a year in limbo as action was delayed and money was spent keeping troubled hospitals afloat. Political expediency made it near impossible to close hospitals where necessary to reconfigure services, as in the case of Chase Farm where the same MP protesting its closure was vehement in his support for national change. The polyclinic concept died a death, although NHS management continued the development of resource centres for primary care where these were needed. The Independent Reconfiguration Panel established in 2003 continued to provide advice to the Secretary of State for Health on contested proposals.
Strategic Health Authorities had been key to reconfiguration until their abolition in 2013, and it was hard to see how major reconfiguration would be driven in future. David Nicholson, before he retired as chief executive of NHS England, said it was not clear who now made decisions. By 2014 it was obvious that hospital policy needed to be reviewed. A situation in which Trusts were divided into FTs and those under the TDA that were waiting to be broken up, merged or radically reshaped, was not appropriate.
Simon Stevens, Chief Executive of NHS England from 2013, saw the provision of care to the many elderly people requiring hospital care to imply the maintenance of medium-sized local hospitals. New patterns of care involving community services and the hospitals were needed. By now NHS England and its regional branches were involved in reconfiguration; proposals to concentrate cardiac surgery in North East London at St Bartholomew’s were pushed through in conjunction with the local CCGs and UCLH Partners.
Naively the orthodox view had been ‘hospitals expensive: bad; primary care cheap: good.’ The quality of the debate improved with the publication of the RCP Future Hospital Commission145 proposing partnerships between primary and secondary care and Simon Stevens’ Five Year Forward View. Stevens said there was triple fragmentation to overcome, health and social care, physical and mental health, and primary and secondary care. Believing that a variety of solutions should be tried, he envisaged more integration of health and social care.146
Unaffected by the result of the 2015 election, NHS England developed teams to trial the models, support and evaluate them. In Primary and Acute Care Systems hospital services would be vertically integrated with NHS list-based GPs and mental health and community services. Multispecialty Community Providers would provide integrated out-of-hospital services, perhaps taking on some specialised hospital work. Viable smaller hospitals would be assessed to examine key services ( for example, see the Dalton Review), and where Trusts had insuperable financial problems, there might be a shared responsibility “for unsustainable organisations across local health communities”. Support for change came from the New Care Models Programme, and the selection of ‘vanguard’ sites.
Factors driving reconfiguration
A multitude of factors influenced the drive to reconfiguration: cost effectiveness, workforce issues, clinical outcomes, pressure to seven-days-a-week working, the development of biomedical research centres and academic health science networks, and the emergence of new centres of power – NHS England and the Shelford Group. Possibly services might be provided more cost-effectively in larger units created by merging Trusts and hospitals. There was little evidence to guide health planners on the ‘optimal’ size of hospitals or indeed on the benefits of reconfiguration more generally. The King’s Fund’s review, The Reconfiguration of Clinical Services: What is the Evidence, showed how little could be expected in terms of savings or, in most fields, improvement in quality of service. One of the most comprehensive assessments of hospital efficiency from the NHS Centre for Reviews and Dissemination suggested that optimal hospital size lay between 200 and 600 beds.147 Normand suggested that there was no good evidence to demonstrate that closing small hospitals saves money, but that merger of particular services (for example, intensive care, A&E services, cardiac surgery) might do so and improve quality.
The real problem is that hospitals are really sheds with workshops inside and not single institutions. There is no evidence that widening the scope of a hospital’s activity leads to lower costs. There is anecdotal evidence that the problems of managing highly complex hospitals increases costs.148
Workforce issues and the impossibility of providing complex staff skills 24/7 in more than a few places were factors. Large mergers were increasingly part of the NHS scene, as some services could not be provided in each and every hospital. In 2016, NHS Improvement allowed hospitals to link, to improve clinical and financial performance and achieve sustainable services. Four Foundation Trusts were accredited: Guy’s and St Thomas’ NHS Foundation Trust, Northumbria Healthcare NHS Foundation Trust, Royal Free London NHS Foundation Trust and Salford Royal NHS Foundation Trust.
The seven-day week hospital
For years evidence had built up, first in the USA and later in the UK, that the outcome of patients was affected by the day and time of admission. Outcomes were poorer at the weekends which led to calls for all hospitals to move to seven-day working and consultant cover. A report published in the Journal of the Royal Society of Medicine analysed all 14.2 million admissions to NHS hospitals in England between April 2009 and March 2010, adjusting for case severity and multiple diagnoses.149 Patients admitted at the weekend were significantly more likely to die within 30 days than those admitted during the week. A 6 per cent spike in deaths in August in the days immediately after newly qualified doctors took up their first post – “the killing season” – led to the introduction of mandatory ‘shadowing’ to mitigate this. Senior staff, and urgent investigations, might not be available 24/7. To have consultants on site at all times reduced mortality, long recognised in obstetrics and anaesthesia, but required a change to consultant working patterns. The RCP supported seven-days-a-week working, as did NHS England in its Five Year Forward View.150 The Medical Director of the NHS, Sir Bruce Keogh, established a forum to examine and report on 24/7 working, perhaps with sanctions on Trusts not providing this. Laboratory and technical services would need to work differently, and GPs and social care had to be available for patients leaving hospital.151 Increasingly hospitals began to work in this way. Inevitably costs would be higher and this might drive hospital closures and mergers, for it would be difficult to deliver seven-day care in smaller hospitals. Coupled with 24/7 working was a belief that, nationwide, A&E departments would have to work in a hierarchical way, with comparatively few dealing with the small minority of cases requiring many different professional skills, and a larger number dealing with most cases. In Northumbria, a new “emergency only” hospital was built in 2014 so three A&E departments at smaller hospitals could close; this would mitigate the problems of 24-hour staffing. However, really major trauma patients would still have to travel to Newcastle.
Included in the election manifestos in 2015, the policy became a key focus for the incoming Conservative government that decided to re-negotiate the consultant contract so that those newly appointed could not opt out of weekend work. A similar attempt to alter the balance of pay of junior doctors so that they earned more during the week and less at weekends brought them to threaten strike action. The costs of seven-day working added to the dire financial situation of many Trusts and led to the allocation of an additional £4 billion in the autumn of 2015.
Biomedical Research Centres (BRCs) and Academic Health Science Centres (AHSCs)
Since the time of William Osler and the Flexner report a century earlier, there had been recognition that service, teaching and research were mutually supportive. Driven from a research standpoint by Professor Dame Sally Davies (the Department of Health’s Director General of Research and Development, and later CMO) the UK government recognised the economic, financial and clinical advantages of supporting medical developments and research leading to better treatment. The example of major biomedical research centres (BRCs) in the USA, which had spearheaded clinical development, led to the establishment of the National Institute for Health Research (NIHR) and consideration of which centres should be supported to encourage “translational research”, transferring the results of research to patient care. Under Sally Davies’ leadership, efforts were made to establish a consistent policy and framework to embed research within the NHS. The NIHR worked in partnership with SHAs, Trusts, and NICE. Its goals were to establish the NHS as an internationally recognised centre for research excellence, attract, develop and retain the best research professionals to conduct people-based research, commission research focused on improving health and social care, strengthen and streamline systems for research management and governance, and act as sound custodians of public money for public good. It was also hoped that the centres would, through their research and development efforts, generate national wealth. The money deployed was NHS research funding, and it therefore went to the NHS Trusts identified. They would receive substantial sums to translate fundamental biomedical research into clinical research that benefits patients, and be early adopters of new insights in technologies, techniques and treatments for improving health. The BRCs would drive innovation in prevention, diagnosis and treatment, translate research into benefits for patients, and contribute to international competitiveness. A series of government publications supported the strategy, Innovation for Health and Wealth, Investment in UK Health and Life Sciences, and Strategy for UK Life Sciences.152 BRCs tended to specialise, UCL Partners, for example in cancer, cardiac metabolism, infection immunity and inflammation, and neurosciences.
A panel of international experts chose centres in open competition as world class in research. In December 2006, Patricia Hewitt, the Secretary of State, announced five multispecialty Trusts that would be supported – three in London (Kings, UCLH and Imperial) plus Oxford and Cambridge, and a further six in particular clinical fields.153 The Medical Research Council (MRC) had major commitments to all the centres. London centres received a third of MRC grants, but Scotland as a whole got 13 per cent and planned to cluster all its research and teaching hospitals into a single centre. NHS research moneys went preferentially to these Trusts, power houses of translational research, and in 2011/12, a second competition identified 11 centres.154
Academic Health Science Centres (AHSCs) followed Ara Darzi’s proposals in his 2007 strategy for the future of the NHS, High Quality Care for All. Sponsored elsewhere in the Department and strongly supported by the PM Tony Blair, Alan Johnson, announced in March 2009 that, after a separate peer review of the final applicants by an international panel of experts, five would be created in England.155 The keynote would be collaboration between a Trust or Trusts with a university. The successful centres were Cambridge University Health Partners, Imperial College, King’s Health Partners, Manchester AHSC, and UCL Partners. From the outset, the AHSCs behaved differently. Imperial behaved imperially, centring power on the university with a single chief executive for the NHS and university sides. Equality between the partner Trusts and the university was the ethos at UCL Partners. These large centres began to play a major role in structuring local and specialist health services.156 While having no managerial authority over the NHS, their influence was considerable. Hospitals in a relationship with universities not selected began to consider their own future and seek links.
Academic Health Science Networks (AHSNs) were launched by the Prime Minister in December 2011. AHSNs enable academics, health care professionals and industry to work together to speed up delivery of cutting-edge medical research into routine practice in the NHS. Designation as an AHSN brought additional money to the organisation. AHSNs provided a platform on which the NHS and academia could work together with industry to identify the most promising innovations and help them to be introduced quickly and widely. Networks, designed to assist in the translation of advances into clinical care, received additional money to assist this. In 2013, the number of networks was expanded to 15, covering the whole of England.
The Shelford Group
A premier league of Trusts emerged from 2011 onwards. They were large teaching Trusts and major research centres. Clinically their performance was very good and their chief executives had been in post far longer than average. Their ten chief executives had nearly 200 years of experience between them and met regularly to discuss issues of common concern. They developed a website, and subgroups of their medical directors and chief nurses were formed. They included Cambridge, Manchester, Guy’s/St Thomas’, Imperial, Kings, Newcastle, Oxford, Sheffield, UCLH and Birmingham. Most, but not all, were FTs. They were important tertiary centres and had common interests not shared by most other Trusts, not least the high costs of the extremely complicated cases with which they dealt. They associated as the ‘Shelford Group’ after the village where their chief executives first met. While not thinking as one, they were a group of incredible significance and were sought out for their views by senior politicians and managers, seeing themselves as a backbone of the NHS, stable in times of instability, and possibly a focus around which the NHS more generally might be organised. In other words, they might be prepared to absorb failing Trusts.157
In 2015 some, including Imperial, rejected the tariff settlement for the coming year because, said the chief finance officer of QE Birmingham, ”Savings of this magnitude and this timescale can only come from the biggest cost centre and that is staffing, mainly nurses. Reduce staffing and you jeopardise safety and quality. All roads lead back to Mid-Staffs.” If they didn’t make savings, Monitor would put them into Special Measures. If they did, quality would fall and the CQC would do the same.
Medical education and staffing
Concerns over the pattern of medical education were expressed nationally and internationally. In 2009, the GMC updated Tomorrow’s Doctors, its guidance on the undergraduate medical curriculum.158 On the international scene, a Commission was established by The Lancet, supported by the Bill & Melinda Gates Foundation, the Rockefeller Foundation, and the China Medical Board.159There was a desire to widen access routes into medicine. A growing number of medical schools offered a four-year fast track course for applicants who already had a degree. However, when the BMA updated its 2004 study on medical school entry, it considered that access had become more inflexible over time. The majority of medical school students were still drawn from professional and managerial backgrounds. The age, ethnicity and gender profile of medical school students raised questions about the structure of medical education and about the future composition of the profession.
24 Medical schools in England, by region and target student intakes (English total 6,195)
Source: HEFCE160
East Anglia
Cambridge (University of), School of Clinical Medicine (299)
University of East Anglia (168)
Greater London
Queen Mary College – Barts and The London (324)
King’s College London School of Medicine (at Guy’s King’s College and St Thomas’ Hospital) (415)
Imperial College School of Medicine, London (330)
London School of Hygiene & Tropical Medicine (Postgraduate medical school)
St George’s, University of London (264)
University College London, University College Medical School (330)
Midlands
Birmingham (University of), School of Medicine (385)
Keele University, School of Medicine (129)
Leicester (University of), Leicester Medical School (245)
Warwick University of), Warwick Medical School (178)
Nottingham (The University of), Faculty of Medicine and Health Sciences (336)
North East
Durham (University of), Queens Campus, Stockton, Phase 1 Medicine
Hull York Medical School (141)
Leeds (University of), School of Medicine (263)
Newcastle (352)
Sheffield (The University of), School of Medicine (241)
North West
Liverpool (University of), Faculty of Health and Life Sciences (371)
Manchester (University of), Faculty of Medicine and Human Sciences (380)
South
Brighton and Sussex Medical School (138)
Oxford (186)
Southampton (University of), School of Medicine (246)
South West
Bristol (University of), Faculty of Medicine (256)
Peninsula Medical and Dental School (216)
In 2014/15 a new private medical school opened at the University of Buckingham, to use the facilities of Milton Keynes Hospital. The Dean was Professor Karol Sikora and the curriculum was based on the University of Leicester’s MB ChB programme. Medical schools frequently admitted more than their target numbers. The target from 2006–2010 was 6,195, but each year more were admitted. In addition, students qualifying elsewhere in the European Community had equal rights to apply for jobs in the NHS. In 2012, a further review projected a significant oversupply of doctors (perhaps by 10,000 by 2025), and a reduction of 2 per cent in medical school intakes was proposed. Yet the rising demands on the NHS, the desire to operate hospitals on a seven-day basis and industrial action prompted the government, in 2016, to commit to expansion of English medical schools by 1,500 places from September 2018. Five new medical schools were announced in 2018 for Edge Hill University in Lancashire, Anglia Ruskin University, Sunderland, Lincoln and Nottingham, and Kent and Canterbury. New systems of modelling that looked at population numbers, levels of need, levels of services and productivity were used. The additional costs that medical education imposed on teaching hospitals had been recognised for 30 years by the NHS.
The costs for medical training (including related clinical placement costs allocated to the NHS) are high, so any expansion of places is centrally planned and financed to meet NHS needs. Intake to English medical schools increased from 3,749 in 1997/98 to over 6,400 in the academic year 2010/11. A review of the total English medical school intake in 2006 suggested that it was now around the right number. There were a total of 28,329 total medical (clinical and pre-clinical) full-time undergraduates in 2008/09. This resulted in an increase to the number of doctors graduating to around 5,684 in 2008/09.
The Medical Service Increment for Teaching (SIFT). In the older medical schools, SIFT could be considerable, £25 million to a teaching hospital. There had been little or no auditing of these sums and the money passing to the central teaching hospital could be much higher than that going to other peripheral hospitals, also with substantial teaching commitments. As part of the allocation system, there was a change to the way SIFT (and MADEL, the levy for junior doctor training) worked, setting a sum for each student for each week in placement, to make the system more transparent and more fair across the country. The cost of a medical education to the students themselves was reviewed and, in 2011, it was decided that support would provide new students with a non-means-tested grant of £1,000, a means-tested bursary of up to £6,000 (varying on income, location and whether the student lived at home), and a reduced rate non-means-tested loan.
The postgraduate training system
In August 2009, the European Working Time Directive came into force, limiting the average hours worked by junior doctors to 48 per week. Concerns soon emerged, including the running of the service, patient safety and the reduction in training experience. The Presidents of the Royal Colleges expressed anxiety about patient care as the teams that were rostered took over from each other. As doctor succeeded doctor on shift systems, patients had to repeat their histories. With restricted hours and increased commitments to education rather than service, who kept the service running? Would competence be acquired under the new system? “Surgery is a body-contact sport; there is no question about it. You can’t be a good armchair surgeon”.161 Nor did juniors always have the skills of their predecessors; when medical students no longer delivered babies, a new house officer who had never done so, (or had never stitched a tear) was not a great help.
Responding to Sir John Tooke’s inquiry into Modernising Medical Careers (MMC) the Department of Health set up a new advisory body. NHS Medical Education England (MEE) was established in January 2009 to provide advice on training and education for doctors, dentists, health care scientists and pharmacists. It was a non-departmental public body supported by a secretariat from the Department of Health. Not quite that proposed by Sir John Tooke, it would be concerned with postgraduate training and would relate to the GMC, which took over the responsibilities of the Postgraduate Medical Education and Training Board in April 2010. The Secretary of State asked MME to review the effect of the European Working Time Directive on the training of junior doctors and the concern that the introduction of a 48-hour working week might have a detrimental effect. MEE asked Professor John Collins, visiting professor in Oxford University’s Nuffield Department of Surgery to evaluate the medical foundation programme. The report in October 2010 raised questions over key aspects of design, content, safety and quality. Some trainees were asked to practice beyond their level of competence and without adequate supervision, placing patients at risk and giving the trainee the impression that suboptimal care was condoned. Further, the system meant that more locums had to be employed to fill gaps at a cost of hundreds of millions of pounds.162
Medical staffing
Trusts needed senior staff and hundreds of posts were created, largely unregulated, often temporary with short-term contracts and with little development/educational support provided. In addition were Associate Specialists, numbering over 3000, often over 50 years of age, senior doctors with significant experience and skills able to work independently at consultant level, contributing equally to on-call rotas and supervising trainees. Though responsible to a named consultant they worked independently. There were also specialist doctors, some 4,000, with lesser training and a salary below that of associate specialists.
The long-standing aim of “a consultant led service” remained a distant prospect. While for 15 years the number of consultants had expanded at 4-5% annually this would not be enough. More juniors were being employed as the European Working Time Directive came fully into force in 2009. With their shorter hours and educational commitments, they might not represent value for money compared with other ways of providing care, and Trusts might not be so keen to have so many junior staff in the future. Hospitals had previously received virtually all the salary of junior staff in training who required almost continuous supervision, but the money hospitals received for this fell. Balancing the numbers in training and job opportunities had been a problem since the start of the NHS. The King’s Fund published a detailed review of its history and problems in 2009.163
The aim of doctor self-sufficiency, to avoid the need of the NHS for overseas graduates, had been achieved by the increase in medical school entry. However, doctors from overseas could compete on level terms with those trained in the UK, and it was likely that the economic downturn would limit the expansion of medical staffing in the NHS. The labour market for doctors looked set to become much harsher.164
In 2016 negotiations over a new contract for junior doctors, designed to make it easier to attain good cover at weekends and move towards safe seven- day working, led to industrial action and strikes. Doctors’ morale was low for many reasons: dissatisfaction with training, rising workloads and financial stringency. A toxic attitude between the BMA and government developed; agreement with the profession was reached following concessions on both sides, only to be rejected by doctors in training. A series of strikes took place which, in the view of many, including senior professionals, undoubtedly harmed patients. Evidence emerged of left-wing politics influencing some of the doctors’ leaders. Ultimately the new contract was accepted.
Women in medicine
The increasing number of women entering the medical profession, likely to form the majority within ten years, made it important to consider the effect on the NHS. The RCP published a report in 2009 on Women in Medicine: the future.165 The report said that women had a far greater preference for part-time and other forms of flexible working and, on average, preferred specialist fields that offered more ‘plan-able’ working hours and a relatively greater amount of patient interaction. Women made up 40 per cent of all doctors, 42 per cent of general practitioners, and 28 per cent of consultants. Women made up 44 per cent of appointments of GPs and in paediatrics, and almost 49 per cent in public health. Only 8.4 per cent of consultant surgeons were women. The differential pattern of female preference for particular specialties was not just a UK phenomenon. These preference rankings were closely matched internationally across a range of diverse health care systems. Follow up of doctors for 15 years after graduating suggested that women provided 60 per cent of a full-time equivalent doctor, against 80 per cent for men.
Nursing
The Prime Minister’s Commission
A wider and wider range of jobs were coming nursing’s way. In 2009, Gordon Brown established a Nursing Commission chaired by Ann Keen MP, a Minister and a nurse. Brown told the Royal College of Nursing (RCN):
Nursing has become even more central to the future of both health care and all our fabric of social life in our country. Nurses are now performing operations ...are now prescribing ... running services... as managers, nurse consultants, nurse practitioners, and ... we want nurses to be more involved and more central and more in control of what happens in the health service in the future.
The Commission would:
...look at all the trends and all the changes and all the forces at work that are going to change our society and also change nursing in the years to come...and take the next steps to enhancing... and improving the status of nursing in our country for years to come.
Ann Keen said that, 37 years after the Briggs Report, the Commission aimed to usher in a new era that located nursing, midwifery and care issues in a central position in policy-making and management. “We will tell a new story about the future nurse and midwife, to create a modern, realistic but inspiring public image.”
Anne Marie Rafferty, Dean of Nursing and Midwifery, King’s College London, wrote: “We need to raise the bar in nursing and midwifery education, practice and research, rooting out poor performance and standing up for standards”.
The vision of the Commission was “that all nursing and midwifery staff fulfil their potential to help people who use NHS services, families and communities achieve the best possible health and wellbeing...”
Front Line Care was published in March 2010, attracting little media comment.166 It was positive and dealt with the nursing profession’s aspirations; to be “placed centre-stage” to address the needs of the growing elderly population and those with chronic conditions, and to return ward sisters to a visible position of authority as part of an overhaul of nursing and midwifery. Some problems and shortcomings of nursing were acknowledged but rapidly passed over, not directly addressed. It largely ignored the public perception of the problems of the recruitment and retention of quality applicants who could communicate well, do their maths, and be kind and caring; and the results of a nursing course that often did not turn out nurses ready for the major responsibilities that would fall on their shoulders.
The report recommended protection of the title ‘nurse’, with only those registered by the Nursing and Midwifery Council (NMC) allowed to use it – even though much, if not most, nursing was now undertaken by HCAs, including such tasks as blood pressure checks. HCAs should be more carefully regulated. It recommended a new pledge for all nurses and midwives stating their commitment to, and accountability for, high-quality and continuously improving care. The report also stressed the importance of skilled midwifery to meet the challenges of a rising birth rate and persistent health inequalities, and strengthening the role of the ward sister.
Nurse education and staffing
The number of nurses registering in England rose slowly. In 2009 there were 561,443 (698,653 headcount) registered nursing, midwifery and health visiting staff:. 57 per cent were qualified and, of these, 6.3 per cent were midwives, 2.5 per cent district nurses, 2.6 per cent health visitors and 3.6 per cent registered children’s nurses. The number of qualified nursing, midwifery and health visiting staff increased by an average of 2.6 per cent per year between 1999 and 2009. The number of overseas nurses registering at first fell, then rose as a necessary recruitment campaign exposed shortages. Trusts, anxious to achieve FT status, had trimmed nurse numbers to save money, and this rolled into recruitment forecasts and cascaded into planning and a reduction in the commissioning of training places. Following the problems at Mid Staffordshire and the recognition that low levels of nurse staffing were dangerous, Trusts hastened to improve staffing, and shortages were inevitable. The immediate solution was recruitment from European countries with an employment crisis and health services in melt down, such as Portugal, Spain and Italy. Nursing intakes to universities were allowed to rise, and though there were enough applicants (some 19,000 students were accepted annually) this could not solve immediate problems.
Over their three-year training, there were 55,000 nursing and midwifery students, of whom 17,000 qualified annually. With Project 2000 there had been a common core year for each branch of nurse education, adult, children, mental illness and learning disability. With new NMC educational standards, students selected their chosen field at the beginning of their course and, though supernumerary, they now had clinical placements almost immediately, which helped retention as students wanted clinical contact. An accent was now placed on supervised nursing, graded to the experience of the student. Students were increasingly allocated to a “host hospital” so that they could identify with an institution, but nursing colleges now stressed the community side of nurse education as never before. Students of adult nursing, children, mental health and learning disabilities all had their placements. Mental health students might work with a charitable crime reduction initiative in the community, a children’s hospice might be used for future children’s nurses, and general practices were encouraged to take nursing students (for which they were paid £15 a day, less than for a medical student attachment). Early experience of nursing in the community might make recruitment to community posts easier in the future.
In November 2007, the government and the NMC launched a review of pre-registration nursing education to ensure that all nurses of the future were equipped to work in a modern health care environment. The consultation was based on a set of draft standards that set out what nursing students must demonstrate to be fit for practice at the point of registration. Some were standards for competence, the knowledge, skills and attitudes that graduate nurses needed to demonstrate at the point of registration. Others were standards for education that pre-registration nursing programmes must meet, relating to the teaching, learning and assessment of nursing students. The issue was an international one. A seminar at the Robert Wood Johnson Foundation saw four realities: (1) more nurses are working outside of hospitals as care shifts formally and informally into communities; (2) evidence that could assist practice is growing rapidly, but is not well-integrated into either education or practice; (3) the need for nurses to effectively work in and lead teams is increasing; and (4) numbers alone will not fill the widening gap between the supply of nurses and the growing need for their services – additional research and new knowledge will be required. Diversity of workforce and patients was an additional issue.
Nurses were being asked to care for more people with complex multiple geriatric syndromes which involved more than keeping these patients alive – it’s helping people live their lives to the fullest extent possible. Organisations also expected nurses to perform at a higher level, to participate and contribute to the quality and safety agenda of the organization.167
In 2009, government, in agreement with the NHS and the nursing professions, said that in future all nursing students would undertake degree courses meeting new standards to be developed by the NMC. The RCN thought this “an important and historic development.” A new syllabus based on the new 2010 NMC standards was introduced in 2011 in many universities and, from September 2013, all entrants were on degree courses. Whether it would make nursing more or less attractive as a profession was hard to say. Few hospitals knew the proportion of their present nursing workforce with a degree, though nationally about a quarter of nurses had degrees.
The huge NHS nursing force required many of each year’s cohort of young people who had many other careers open to them, but mature entrants were now commonplace. Recruitment was hard and many student nurses were in their late twenties. Project 2000 had aimed to professionalise nursing by encouraging greater academic involvement with university diploma courses and degree courses. The aims of nursing education included the development of nurses as people with enquiring minds. University nursing courses varied significantly in the quality of their intakes and in the percentage finishing their course, although NHS London research showed that most students who left did so because of their experience in practice, not in the universities. At one London course, only 8 per cent completed training. NHS London, the SHA, wished for new, higher-quality standards for the training, reduced the number of student places and chose eight preferred universities eligible for the £61 million training contracts, with the aim of improving the quality of care given to patients. It was responding to two problems: a reduction in the training budget, and issues of quality. Professor Trish Morris-Thompson of NHS London said the move was “in response to concerns from the nursing profession about the quality of the product coming out of the Higher Education Institutions.” “Nurses were graduating who weren’t employable, there were issues around literacy, numeracy and attitude,” she said. “We want to drive up the quality of training to make sure they can contribute to the workforce and are employable.” A London Trust chief executive said that a third or more of applicants routinely failed basic tests of literacy and numeracy.
In April 2012, the RCN established a commission, chaired by Lord Willis, because of growing concern about the performance of nurses, particularly in the care of the elderly. It asked what were the essential features of pre-registration nursing education in the UK, and what types of support for newly registered practitioners are needed to create and maintain a workforce of competent, compassionate nurses fit to deliver future health and social care services? The commission dealt with the theory of nurse education rather than with the quality of nursing within the NHS. Reporting in November 2012 the commission found no evidence that linked the pattern of nursing education with poor standards of care, encouraged the move towards a graduate nurse force, and the mandatory regulation of health care workers.168
“Second-tier nurses”– for example, the old state-enrolled nurses (SENs) had always been important, and might be more so in the future. Camilla Cavendish, in a report for government on HCAs, concluded that:
as the 1946 model of ‘diagnose, intervene, cure’ gives way to the twenty-first century reality of ‘diagnose, intervene, live with a chronic condition’, society urgently needs a flexible, caring workforce with a common base of values and knowledge. While the actual skills required will always vary between settings, junior workers in health and social care are increasingly going to need to draw on similar core knowledge and approaches. If we can bridge divides between health and social care, and between assistants and nurses, we can reduce costly duplication, create a more effective workforce, and raise the status of caring.169
When student nurses ceased to be on the Trust establishment, and with the abolition of the previous SEN training system, the gap was filled by HCAs - there were roughly 250,000 supporting doctors and nurses in the NHS and over a million providing care in total. For every four registered nurses with either a diploma or a degree, there were at least two HCAs. At ward level, a ratio of six qualified staff to four HCAs provided a benchmark. Because HCAs were not registered, there was no central mechanism to deal with complaints against individuals. Some colleges and hospitals took the training of HCAs seriously for it was likely that the demand for a second-tier nurse would grow and much basic nursing would continue to fall on their shoulders.
Quite as important was the need to terminate training when practice fell short, regardless of an individual’s academic ability. Assessment of student attitudes at an early stage of their course was important, as was mentoring and support, in the interests both of the student and the patients. Some universities withdrew nursing students from placements where the support to students was poor.
Although 50 per cent of student nurses’ three years is spent in practice, in 2011 Peter Carter, Chief Executive and General Secretary of the RCN, said “many new nurses arrive in hospital incapable of caring for patients because they have spent too much time in the classroom and not enough on the wards… the NHS was becoming increasingly reliant on unregulated and untrained HCAs to do basic nursing.’170 A hospital in the Midlands explored whether it would be possible to bring back a hospital-based nurse training school, failing to accept that practice already represented 50 per cent of student time.
Nursing practice
The importance of the role of the ward sister was increasingly recognised, for she was in a leadership position and in the best place to ensure that the basics of nursing care were right. Perhaps the most practical initiative of the decade was ‘The productive ward, releasing time to care.’ A national project, it encouraged all on a ward to examine how they worked, how the pattern could be improved, how storage systems and the basic activities on a ward could be made more efficient, so that more time was available for direct nursing care. With proper leadership, both at ward and hospital level, some 10 per cent of nursing time could be saved.171 Other mundane improvements, for example, using a red tray to serve meals to patients who had difficulty in feeding themselves, could have a dramatic effect. Every nurse could see whether such patients were coping and could help them if they were not.
In line with the attempt to measure the quality of care, stressed in the Darzi reports, Alan Johnson, the Health Secretary, suggested that, in the nursing field, treating patients with compassion, reducing the number of falls on wards and good hand-washing were the indicators that could be used to measure the quality of nursing care in the NHS. Safety could encompass indicators such as the number of falls on a ward or infection rates. Compassionate care – whether patients are treated with compassion and whether they are fully kept informed of what is happening with their treatment – and effectiveness, including patients’ nutritional state, minimisation of pain and results of hand-washing audits all needed to be monitored. An increasing number of reports stressed the need for compassion and caring. Research also showed that the level of nursing support, and the education of the nurses, had a major influence on patient survival. Lower mortalities, internationally, were associated with higher nurse ratios and nurses trained to degree level. NHS England commissioned from Professor Alison Leary a detailed analysis of high-quality data available at the Coventry and Warwickshire Trust. For the first time, a good analysis was available from English data of the relationship between the proportion of registered nurses on the ward and indicators of quality such as patient falls.172
The 2009 Report from the Patients’ Association, Patients Not Numbers, People Not Statistics, showed from individual patient’s stories how far the NHS had to go.173 In February 2011, the Health Service Ombudsman, Ann Abraham, reported that the NHS was failing to treat older people with care, compassion, dignity and respect. The report, Care and compassion?, based on the findings of ten independent investigations into complaints about NHS care for people over the age of 65 across England illuminated the gulf between the principles and values of the NHS Constitution and the reality of being an older person in the care of the NHS in England. How far was this a problem arising from the educational system?
In January 2012, David Cameron, the Prime Minister, unveiled a package of measures designed to tackle “the real problem” with standards of nursing care. The Francis report was giving support to nursing. Nurses would be told to do regular ward rounds and patients encouraged to carry out inspections as part of a drive to improve standards. Central to the plan was the ‘Time to Care’ initiative, to improve efficiency and reduce paperwork so that more time was spent with patients, and a new quality forum would be established. Regularly chief nurses continued to launch initiatives to bring compassion more centrally into nursing. A Safe Staffing Alliance Statement, coming from the King’s College in 2013, said that a ratio of more than eight patients per registered nurse significantly increases the risk of harm and constitutes a breach in patient safety. The following year, draft NICE guidance said that hospitals should be wary about having nurses care for more than eight patients each on wards during the day.174
Nurse practitioners
With pressure on health care costs worldwide, senior nurses in the USA wrote in the New England Journal of Medicine that it was essential to use all “health care providers” to the maximum of their capabilities.175 A growing shortage of primary care providers seemed to ensure that nurses (nurse practitioners) would ultimately be required to practice to their fullest capacity. Evidence from many studies indicated that services, such as wellness and prevention, diagnosis and management of many common uncomplicated acute illnesses, and management of chronic diseases such as diabetes could be provided by nurse practitioners at least as safely and effectively as by physicians. In many states, independent practice and prescribing was permitted though there was opposition from some medical organisations.
The condition of the NHS
As the seventh decade proceeded, the national health service remained, as it had ever been, in turbulent waters. It would probably never return to the comparative calm in which people accepted that the service was hardly to be questioned, and whatever was on offer was to be received with gratitude. Hardly a day passed without a newspaper campaign, from the Mail or The Times, about the care of the dying, of the elderly, maternity services or delays in the diagnosis of cancer. Ministers had attempted to devolve their responsibilities to the service, commissioners or NHS England. Neither the population, nor the political opposition was having it.
Improved efficiency alone, reconfiguring hospital services and Service Transformation Plans, moving care from hospitals into the community and general practice, or bolstering local authority social services, was not going to satisfy the need for care, let alone the demand. Raising taxes might be politically disastrous and economically foolhardy. The stress on those managing or providing the services, from the hospital chief executive to the stressed nurse on the ward, was unrelenting. A distant hope was that, as England moved out of recession, more money might be found for the NHS.
The Times believed that the time had come to think the unthinkable: the pledge that health care should be free at the point of delivery. Across developed nations, insurance-based schemes with co-payments were the norm. Across the board, funding increases were not the answer. To make high-quality health care available to all was the most important. Voices were raising the possibility of charges if it would help to fund better care for all. Others believed such proposals would increase inequalities and reduce access. An honest debate was required, said The Times.176
Jeremy Hunt, the Secretary of State, adopting social media, tweeted about the biggest things that he wished he had known when he took up his post. The top issues were:
a) Importance of detailed workforce planning
b) Critical link between NHS and social care and
c) If you want to improve patient safety, ‘there is no change without culture change...’
d) Reform that moves care models to prevention
e) Grasping potential of tech to transform health, as it has every other aspect of life.