The NHS Long Term Plan has set an ambitious aim of reducing the number of outpatient attendances by 30 million over the next 10 years. In part this is a reaction to the huge growth in appointments and attendances over the last decade, and partly due to possibly better ways of delivering care, reducing inefficiencies and improving patient experience and outcomes.
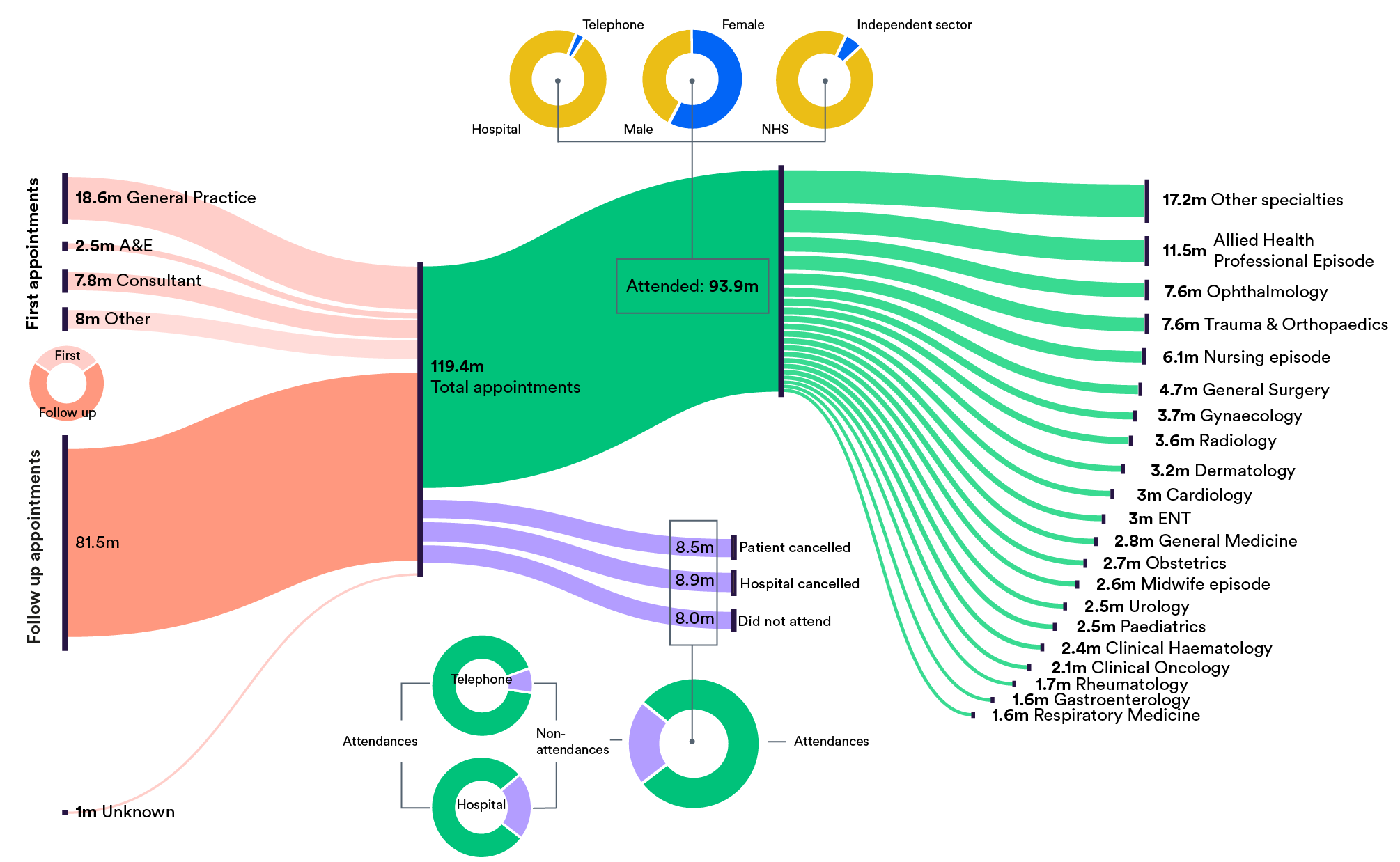
After general practice, outpatient clinics account for the largest number of patient contacts with the NHS each year. As the diagram shows, in 2017/18 there were over 119 million appointments across the English NHS – over two appointments for every person in England. Although this is slightly fewer appointments than the previous year, in the decade to 2016/17 the number of appointments doubled – growing at around 7% per year and far outstripping population growth.
Around two-thirds of all appointments are follow-ups booked in outpatient departments. The remaining 37 million appointments are made by GPs, consultants and other health care professionals, or referrals from A&E departments.
But not all appointments make it through to an actual attendance. As the number of appointments have risen, so too have the number of people failing to attend or cancelling their appointment (or had their appointment cancelled by the hospital). In 2017/18, non-attendances had risen to 22% – up from 18% in 2007.
One reaction to the high number of non-attenders can be a tendency to overbook outpatient clinics. Although overbooking can mitigate some of the problems of non-attendance, it is a crude and not always effective response that can also create its own problems. More sophisticated approaches to making appointments – the use of ‘partial booking’ (to be confirmed near the appointment date), reminder texts/emails and more structured, patient-activated, protocols to trigger follow-ups, for example – can reduce non-attendance and also improve patient experience.
Not all outpatient consultations are made in person of course. In 2017/18 around 2.7 million (3%) were carried out by telephone. Such consultations not only have a much lower rate of non-attendance – 8% compared to over 22% appointments at outpatient clinics – but also reduce travel (and its carbon cost) for patients.
And not all clinics are provided by the NHS. Around 5.5 million attendances (6%) in 2017/18 were paid for by the NHS but delivered by the independent sector. These included not only commercial providers such as Virgin, BMI, Specsavers and Spire, but GP practices and collaborative partnerships between GP federations and NHS organisations.
Of the top 20 specialties by attendance figures, allied health professional episodes accounted for 11.5 million in 2017/18 – nearly a quarter of the 39 million total increase in attendances since 2007.
In fact, just four specialties (allied health professions, nursing, radiology and midwifery) accounted for around 50% of the total increase in attendances over this decade.
The Long Term Plan’s goal to reduce attendance numbers over the coming decade – while improving quality, experience and outcomes – will require, in its own words, ‘redesigned hospital services’, ‘streamlined pathways’, and in particular, ‘digitally-enabled outpatient care’.
While there are local examples of the use of technology – such as video consultations – they are not universal. And although incentivising providers to adopt (and adapt) new ways of delivering outpatient care have been introduced this year through new payment tariffs, in particular for non-face-to-face consultations – NHS trusts still need to work out how best to redesign their outpatient services in response to the incentives they face.