The Covid-19 pandemic has brought into sharp focus the uneven burden placed on patients by long-term health conditions like heart disease, diabetes, asthma or mental ill-health. Higher mortality from Covid-19 in deprived areas is in part related to higher levels of underlying health problems. Not only that, but people with long-term conditions have experienced poorer mental health and increased loneliness during the pandemic.
Even prior to Covid-19, it was clear that people with two or more long-term conditions were the highest users of health care, accounting for over half of hospital admissions, half of general practice appointments and three-quarters of the cost of NHS prescriptions in primary care.
Using survey data from 2018, our new research examines how far primary care and other local services had been meeting the health care needs of people with two or more long-term conditions pre-pandemic. What did our analysis uncover – and how might patients be supported more effectively now and in the future?
People’s needs are not being fully met by their local services
We looked at data from 200,000 patients with long-term conditions registered with GP practices in England to see how far patients’ needs were being met in their last GP appointment. We also looked at whether the support those people were getting from local services (such as community support groups, charities or pharmacies) was able to meet their needs.
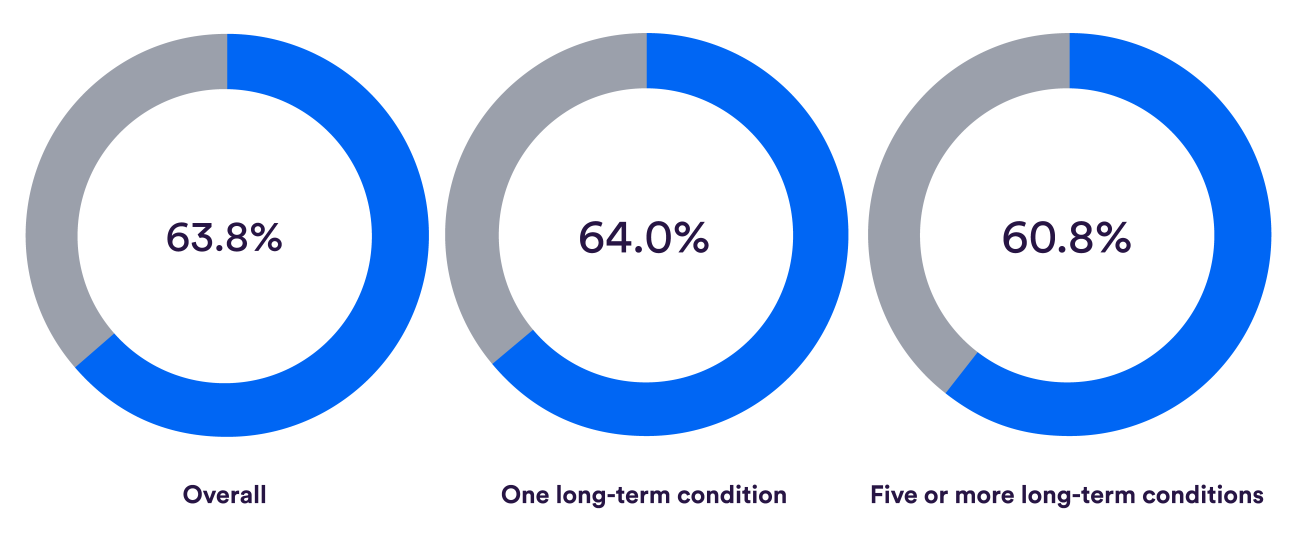
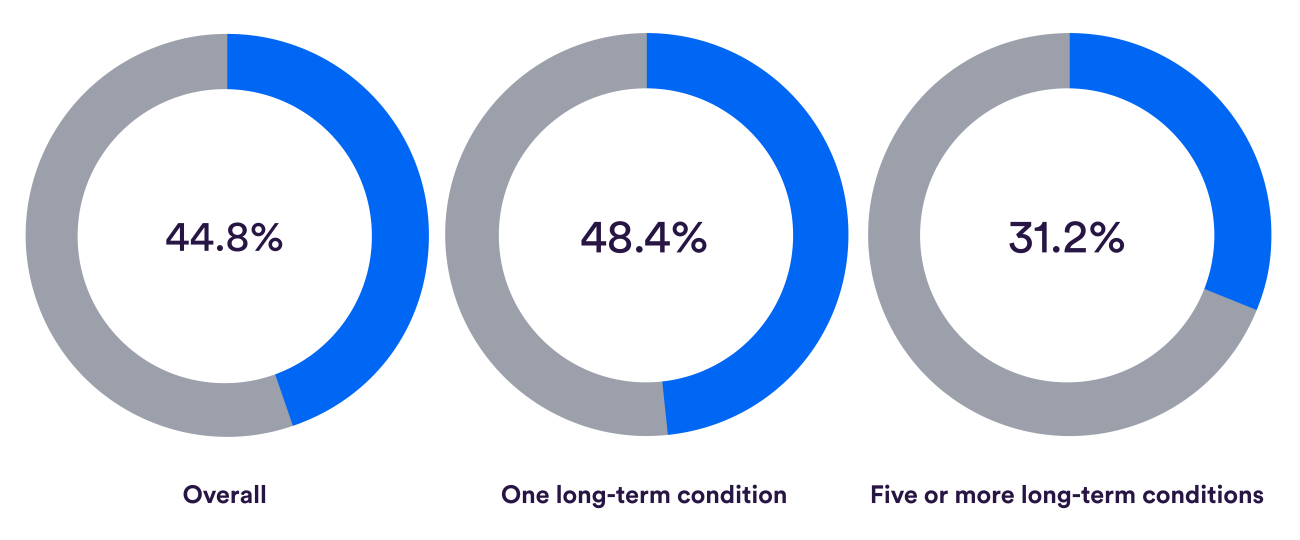
While, overall, patients’ needs were met at their last GP appointment (see first row of charts below), less than half the patients with at least one long-term condition felt they got the support they need from local services – and this fell to under a third for people with five or more conditions (see the second row of charts below).
Among people with multiple long-term conditions, there were groups who were much less likely to have their needs met. After taking account of other characteristics of patients, we found that:
- younger patients, aged 16–24, were less likely than patients aged 45–54 to report having their needs fully met, and less likely to feel supported by local services
- patients of Asian, black and other minority ethnicities were less likely to feel that their needs were met compared with white patients
- patients who felt isolated, frail, or who needed more help with day-to-day activities were also more likely to report their needs going unmet compared to those who did not experience any of these difficulties.
Bucking the trend: can high levels of unmet need be reduced?
Results from the most recent GP patient survey, undertaken from January to March 2020, show that since our analysis, the proportion of people whose needs were fully met in the last consultation fell from 64% to 62%, and those who were fully supported by local services dropped from 43% to 40%. The outlook is getting worse rather than better for the growing number of patients with multiple health conditions.
There are challenges in meeting the needs of people with more complex conditions, and limited evidence about how to achieve this. Part of the difficulty is that although there are established treatments for individual health conditions, and for addressing common risk factors such as obesity, together these place a significant burden on patients. The focus on managing individual conditions in general practice poses a problem for those with multiple conditions, and trying to achieve disease-specific goals for these patients may compromise other aspects of health and wellbeing.
Longer appointment times for patients with complex needs and organising services so that patients can see the same GP have both been recommended to improve care for people with several health conditions. But both of these approaches are harder to deliver at a time when practices are also being tasked with improving access and delivering primary care through larger practices and shared services.
Regarding the use of local services such as community support groups, charities or pharmacies, we were unable to establish whether the unmet need here was a result of patients being unaware of what support is available locally, whether services are hard to access, or whether there are particular services that are not available in their area.
Our analysis found concerning levels of unmet need among patients with two or more long-term health conditions. People with five or more conditions were least likely to have their needs met, either in their last consultation or from local services. The NHS is aiming to deliver more personalised care, particularly for people with complex needs and in deprived areas.
The Covid effect
Covid-19 has exacerbated the challenges already faced by people with multiple long-term conditions, from increased burden of illness and mortality from Covid-19 directly, as well as from reduced access to their usual services, and isolation from family and friends. As the NHS struggles to balance the demands of responding to Covid-19 with maintaining services for other conditions, it will be even more important than before to track whether initiatives such as personalised care bring benefits to patients with multiple health problems.
Suggested citation
Rolewicz L and Scobie S (2020) 'Are the needs of people with multiple long-term conditions being met?'. Nuffield Trust blog.