Multi-professional teamwork in general practice is not new. GPs and nurses have worked together for decades, combining their different skills to address patient needs. But five years ago, the Primary Care Workforce Review acknowledged the long-term shortage of GPs, and concluded that the future of general practice and primary care will depend on greater teamwork between different medical professionals.
To deliver day-to-day services, many practices now employ a range of clinicians – nurses, pharmacists, paramedics, physiotherapists and physician associates among them. Questions therefore arise about how they can all best work together.
A workshop by the Nuffield Trust and the Royal College of General Practitioners, held just before the Covid-19 pandemic, brought together GPs, nurses, paramedics, physios, patients, academics, workforce planners, educators and others to chew over how to develop effective multi-professional team working in general practice.
It highlighted a range of issues that should shape the expansion of teamwork.
Key things to consider
First, there is no universal blueprint. The composition and work of teams must be shaped by local context – not least the shape of the local workforce. Can GPs be recruited in the area? If not, who else is covering their work? What local supply is there of other staff such as pharmacists? Is there a nursing course or physiotherapy course in the area?
Second, what are the health needs of the local population? An inner-city area with a young population is likely to have more mental health and drug and alcohol problem than a coastal retirement town where dementia and incontinence will be more prevalent. With new clinical roles being funded through primary care networks, the choice of who to recruit should be shaped locally, in response to such local characteristics.
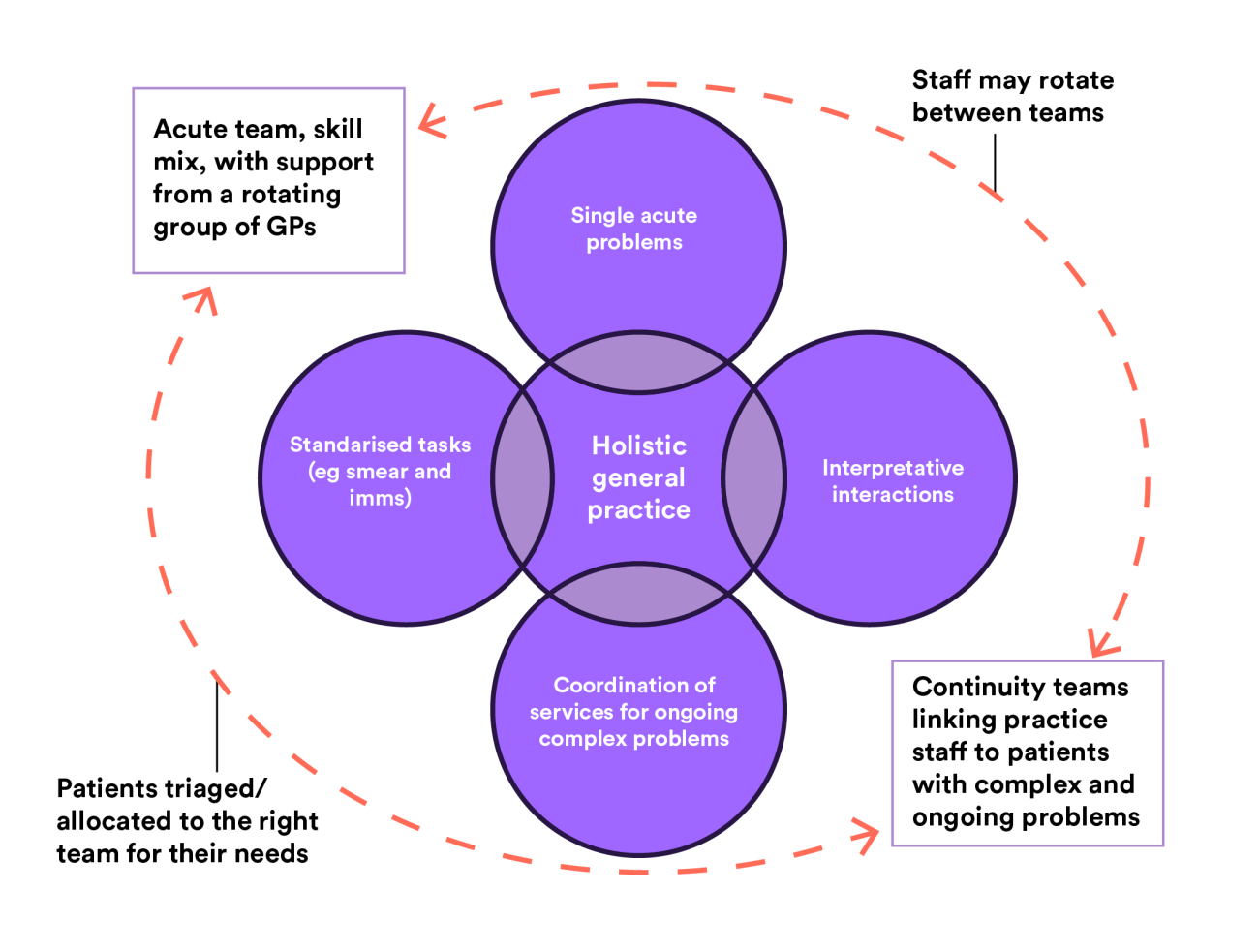
Third, general practice incorporates a wide range of activities (depicted in the purple circles in the image below) and patients’ needs change over time – spanning rapid access for acute problems, predictable needs for things such as immunisations, and repeated access for undifferentiated symptoms or complex ongoing problems.
In addition, the pandemic has created an additional pool of patients awaiting investigations or treatments, such as joint replacements, whose access to specialist care has been delayed. These patients will need a mix of clinical review (to treat ongoing symptoms and prioritise clinical need) and administrative support to help them access scarce hospital appointments.
The teams that emerge in practices or networks must be able to cover these diverse activities and respond in a timely and clinically appropriate way, as the needs of registered patients change over time.
How teams might emerge
Once an appropriate local skill mix has been defined, the next challenge is how to organise it into teams that can balance rapid access, planned appointments, continuity of care, part-time working and more.
The workshop explored two archetypes of how GP teams might emerge. The first deconstructs general practice into different tasks and functions, and teams are developed to respond to specific issues. A network physio clinic for people with joint pains; medication review clinics run by network pharmacists; on-the-day rapid access clinics run by a multi-professional team for acute problems. All could ‘free up’ GPs and nurses to do other things – including care coordination for people with complex needs.
At the opposite end of the spectrum was a model that focused more on the holism of general practice, in which a group of professionals work together in different ways at different times, forming and reforming in different teams to address the broad and changing needs of patients.
Dr Phil Wallek described this matrix way of working when discussing his experience of setting up and refining teamwork in his practice in East Sussex. GPs there are all linked to continuity teams – with a defined group of patients with complex needs – but they also do some sessions in the acute clinic. Locum and retainer GPs who are less able to provide follow-up care do mainly acute clinics.
This flexible approach to team working continues to evolve as they learn from each iteration and seek to improve both patient and staff experience. It avoids rigid segmentation into categories such as ‘healthy’ and ‘complex’ and can respond quickly – though triage and classification systems – to changes in the health and care needs of each individual.
Careful design and implementation is essential
None of these approaches are easy to implement. They need various forms of organisational development support, which are described in an accompanying blog by Simona Baracaia. They highlight that with careful design and detailed attention to operational support, it is possible to preserve the breadth of general practice activities even in the face of workforce challenges. But this should not be at the cost of diluting the holistic, person-centred care at the heart of general practice.
The rapid roll-out of primary care networks and GP contract framework highlight a tendency to enforce national policies and standardise general practice. With thoughtful design and implementation, a growth in teamwork is perfectly compatible with preserving the best of what general practice has to offer, and adapting this to what local populations need.
Rebecca Rosen is a GP and a Senior Fellow at the Nuffield Trust. Professor Martin Marshall is a GP and the Chair of RCGP Council.
Suggested citation
Rosen R and Marshall M (2020) “What should shape the expansion of multi-professional teamwork in general practice?”, Nuffield Trust / RCGP.