The announcement on NHS staff pay nearly raised as many questions as it answered. The initial focus was understandably on whether the headline award was sufficient and how it would be funded. Yet it still remains unclear whether the pay settlement sought to – and has – reflected both cost of living increases and reimbursement for working during the pandemic. In fact, the actual effect on the pay packets of those existing staff who have had to work through the Covid crisis is not obvious from the headline settlement figure. Moreover, how does the settlement affect pay inequalities? This blog explores these issues further.
What was agreed?
The government has accepted the pay recommendations made by the NHS Pay Review Body and the Review Body on Doctors' and Dentists' Remuneration (‘the review bodies’) for staff in England1. The 3% increase for the 1.2 million employed on the NHS terms and conditions of service (Agenda for Change) means that the starting basic pay for a full-time health care assistant or security officer is £541 higher for 2021/22. The equivalent figure is £748 for newly qualified nurses, £1,373 for modern matrons and £2,731 for chief finance managers2.
Doctors are employed on different contracts, including some – such as doctors in training (junior doctors) – who are covered by previous multi-year agreements, and so their pay level was not considered this year. However, the starting basic salary for a consultant, the senior hospital-based physicians or surgeons, will be £2,463 higher in 2021/22.
The figures above do not include non-basic pay such as payments for additional activity, on call and shift work, which will increase as a consequence of the settlement. On average, non-basic pay account for an additional 14% of nurse and 23% of consultant pay (the latter excluding medical awards which have not been increased in this settlement). The increases quoted also do not account for the pay progression that some existing staff are due to reflect their years of service, which is discussed later on.
Does the pay settlement reflect the pandemic?
In reaching its recommendations, the review bodies consider, for example, the need to recruit, retain and motivate suitable staff, as well as affordability and inflation. But this year’s pay settlement is different.
The pay review bodies’ reports, and the Secretary of State for Health and Social Care in accepting their recommendations, allude to the need for the pay settlement to recognise the “extraordinary efforts” of NHS staff during the pandemic and that staff experienced fear from putting themselves and their families in danger. The NHS Pay Review Body then makes the case that “NHS staff pulled together as one team” and imply that the pay of all staff – as opposed to just some professions – should reflect the efforts during the pandemic. Of course, the pandemic did not affect all services and staff groups equally, but given the difficulty and divisiveness of differentiating between roles, having a uniform approach appears reasonable.
But we don’t know what the pay settlement would have been without a pandemic. However, for the sake of demonstrating the difference between pay for various groups, let’s assume the ‘Covid pay’ is the amount over and above expected inflation – accepting, as outlined above, that pay settlements seek to address other factors in addition to inflation – which they predict at 1.7% based on Bank of England forecasts. This is on top of any additional pay that staff have earned since the start of the pandemic for working longer or unsocial hours.
This would imply ‘Covid pay’ being in the region of £230 extra basic pay for a new health care assistant across 2020/21, £320 for a new nurse and £1,440 for an experienced consultant, which represents a six-fold difference based on these indicative assumptions3. And some staff have had no increase over what they already expected, such as junior doctors who are getting the previously agreed 2% increase in pay scales. Some other parts of the workforce – including those cleaners, porters, catering assistants and security guards working for contractors within NHS services – are not covered by this pay setting process.
It is beyond the scope of a blog to ascertain what an appropriate ‘Covid pay’ adjustment should be. However, looking at other professions which have had no let-up in workload4, or may have had some additional risk, gives a mixed picture.
The annual earnings for undertakers, mortuary and crematorium assistants increased by 6% in 2020, for shelf fillers the rise was 7%, and for secondary education teaching professionals it was 2%. The comparable figure for nurses was 1%, although comparisons of average pay between professions should be treated with caution given potential changes in structures of the various workforces.
The other UK nations have all given a flat-rate, one-off payment to health and social care staff – aside from any further consolidated pay settlement. These payments differ somewhat. For example, in Northern Ireland and Scotland (unlike Wales), the level was adjusted for part-time working (i.e. pro rata). The payment was also lower in Scotland (£500) compared to the other two nations (£735). However, all of them were subject to tax, meaning the additional take-home payment would typically be lower for the higher rate taxpayer.
How will pay packets actually be affected?
The impact on the pay of staff who have worked during the pandemic is variable and somewhat confusing, with the “3%” headline not telling the whole story.
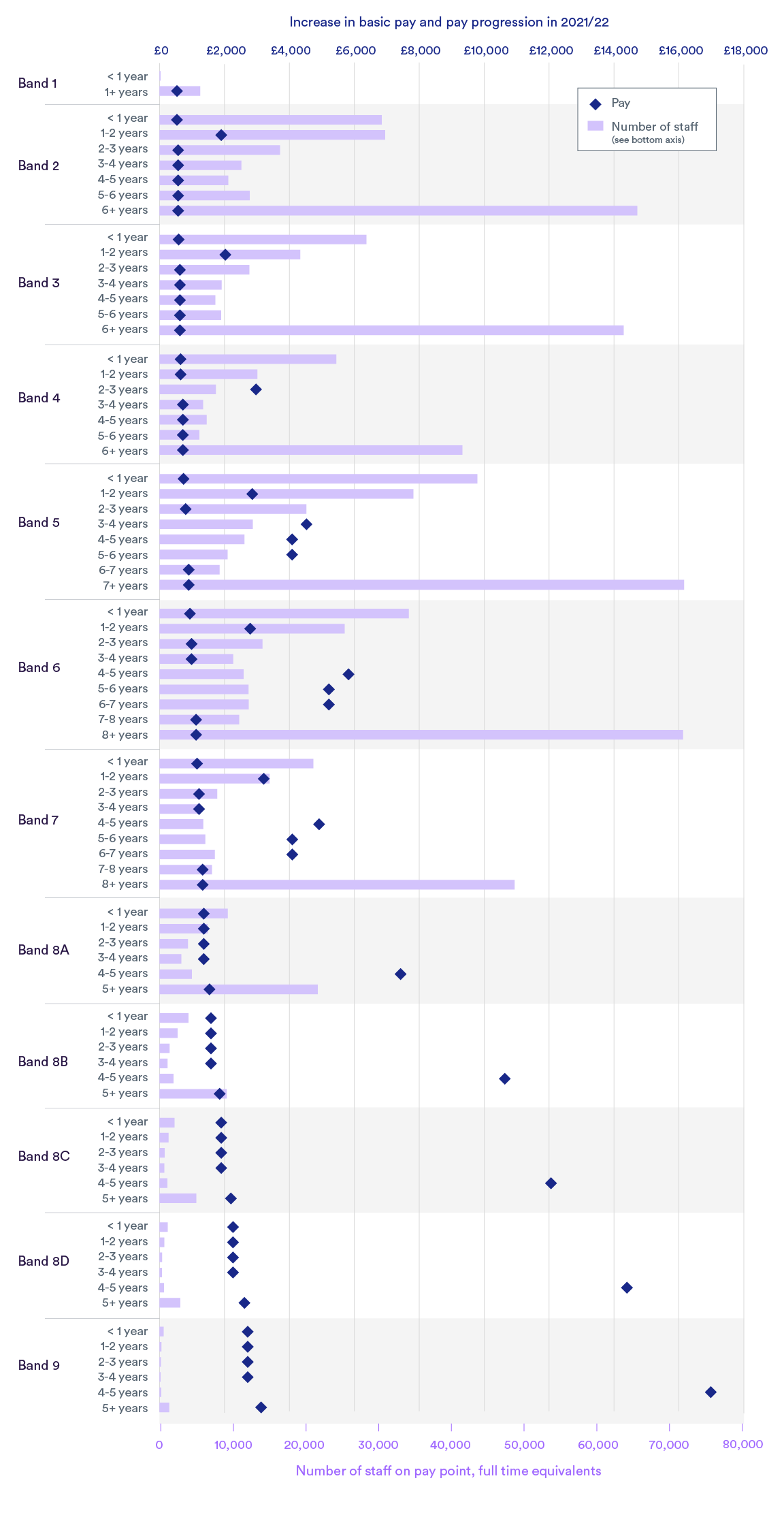
For the largest of the employment contracts, Agenda for Change5, this is because some will move to a higher pay point – worth up to 17% – in recognition of their years of service. Also, for this year specifically, already agreed changes to some of the pay structure mean that some will receive rises worth up to 12%. Around one in five will benefit from this pay progression or restructuring.
In total, while the majority will receive just 3%, the available data suggest that the average increase across all existing staff if they stay is in the region of 5%. The levels of pay increases, and the number of staff due them, are set out in the figure below.
The NHS consultant contract also has pay increments for those reaching certain milestones6. Taking these into account, basic pay for existing consultants will increase by up to 10% or up to £9,419. That said, given this pay settlement does not apply to clinical excellence awards – which account for, on average, a twentieth of earnings but can be worth over £77,000 – many consultants’ total earnings will increase by less than 3%.
What are the implications for equality?
The review bodies’ remits include taking account of the legal obligations on the NHS, such as anti-discrimination legislation regarding age, gender, race, sexual orientation, religion and belief and disability.
While the pay review bodies do summarise the evidence submitted on inequalities, they do not publish an assessment on whether the effect of their recommendations may vary between characteristics. It appears there will be an unequal effect.
This is because, for example, male and white staff are more likely to be in higher paid roles, and so on average receive a higher absolute increase when pay settlements uniform percentages. For example, while the average salary of clinical support staff may increase by around £700, for consultants – which has far less participation from women and those from black and black British ethnicity – the increase will likely be in the region of £3,000.
|
Number of staff (nearest 100) |
Male (%) |
Black and black British (%) |
Estimated annual earnings per FTE, 2020/21 (nearest £100) |
Estimated average proposed uplift per FTE (nearest £10) |
|
|
Support to clinical staff |
414,700 |
18% |
7% |
£24,400 |
£640 - £730 |
|
Nurses and health visitors |
342,300 |
12% |
9% |
£39,100 |
£1,030 - £1,170 |
|
Managers |
22,600 |
38% |
4% |
£56,800 |
£1,600 - £1,700 |
|
Consultants |
54,600 |
62% |
3% |
£127,100 |
£2,940 - £3,610 |
Notes: Uplift excludes pay increments. Minimum uplift calculated as 3% of basic salary, with maximum 3% of annual earnings (excluding medical awards). Staffing levels based on NHS Digital data as at December 2020.
Pay is not everything but it is important
Pay is, of course, not the only way in which the workforce can be valued. Wellbeing support, flexible working, annual leave entitlement, progression opportunities and manageable workloads are all also important. But pay is an important factor and staff deserve a transparent agreement, as do the public as taxpayers and service users.
While having a single, simple percentage increase may be attractive – particularly given past fiascos in communicating pay deals – a failure to disaggregate between Covid-related pay and addressing pre-existing issues with pay levels makes it very difficult to assess whether this is a fair deal. This is not to say there is a practical, easy solution to pay, and there needs to be sufficient variation in pay between roles to reflect, for example, different responsibilities. However, some of the inequalities in the level of increases between staff groups, seniorities and demographics seem questionable, and should be explained by the review bodies and government.
Suggested citation
Palmer W (2021) “After the dust settles: some overlooked and underappreciated aspects of the NHS pay settlement ”, Nuffield Trust comment.