Over half of the UK population born after 1960 will be diagnosed with cancer at some point in their lifetime. Access to timely and effective cancer services is crucial for patient experience and outcomes. Cancer waiting times are a key priority for the Department of Health, and there are currently eight operational standards for cancer care in the Handbook to the NHS Constitution for England. NHS England will begin performance managing Trusts against a new 28-day faster diagnosis standard in April 2020, following recommendations from the Independent Cancer Taskforce. The waiting time targets span the patient pathway, from referral to diagnosis and treatment.
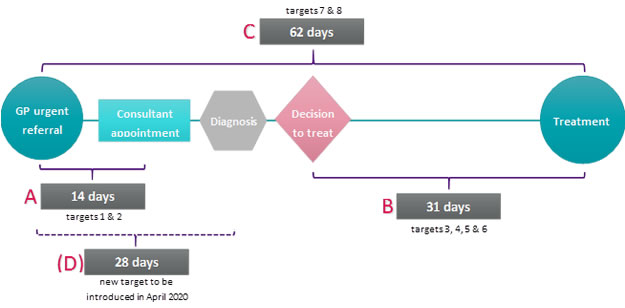
Figure 1 helps to illustrate the cancer waiting time targets, which can be split into four categories:
- A. Two week wait from GP urgent referral to first consultant appointment (for all cancers (target 1) and a separate target for patients with breast symptoms (target 2))
- B. One month wait from decision to treat to a first treatment for cancer (for all treatments (3) and separate targets for radiotherapy (4), surgery (5) and anti-cancer drug regimens (6))
- C. Two month wait from GP urgent referral to a first treatment for cancer (7) (and a separate target (8) when referral is from a national screening service)
- (D). 28-day wait from GP urgent referral to a diagnosis or ruling out of cancer (a new target)
Figure 1. Cancer waiting time targets
Each waiting time target has an associated ‘operational standard’, which is the percentage of cancer patients that are expected to meet the target. We have produced a set of cancer target graphics showing the percentage of patients that breached the cancer targets for each month from 2009 to 2017 in England. The turquoise colours indicate that the target was met, and the pink colours represent a breach of the target. As you cast your eye across the charts, the colour gradients illustrate how access to timely cancer care has changed over time.
2.1 Two week wait from GP urgent referral to first consultant appointment
The two week wait from GP urgent referral to first consultant appointment target has been met in all but two months since 2009. Despite this, the chart indicates that overall performance against the target has decreased over time. Between 2010 and 2013, the average proportion of patients breaching the two-week target each month was 4.4%, but this increased to 5.8% between 2014 and 2017.
2.2 Two week wait breast symptomatic (where cancer not initially suspected) from GP urgent referral to first consultant appointment
Performance against this target has varied considerably from month to month. When the target was first introduced in January 2010, 11.8% of symptomatic breast patients waited longer than 14 days to see a specialist following urgent GP referral. Timely access to a consultant appointment subsequently improved, and from 2011 to 2013 the operational standard was consistently met. Since April 2014, the target has not been met in 20 out of 44 months.
2.3 One month wait from a decision to treat to a first treatment for cancer
This cancer waiting time target has consistently been met, although there has been a slight worsening of performance over time. Prior to 2014, generally between 1% and 2% of patients waited longer than 31 days to start cancer treatment following a decision to treat. Since 2015, over 2% of cancer patients have had to wait more than one month to start treatment.
2.4 One month wait from a decision to treat to a subsequent treatment for cancer (anti-cancer drug regimen)
2.5 One month wait from a decision to treat to a subsequent treatment for cancer (radiotherapy)
2.6 One month wait from a decision to treat to a subsequent treatment for cancer (surgery)
The previous three one month cancer waiting time targets have been met every month since their introduction (apart from January 2015 when the surgery target was not met). The proportion of patients waiting longer than 31 days for an anti-cancer drug regimen has been consistently low, fluctuating at less than 1% in all but three months since 2009. There has been a slight worsening in adherence to the radiotherapy and surgery waiting time targets over time. In November 2017, 4.5% of patients waited over one month for cancer surgery, compared to 2.7% in November 2011. The proportion of patients breaching the radiotherapy waiting time target increased from 1.2% to 2.5% in the same time period.
2.7 Two month wait from GP urgent referral to a first treatment for cancer
Nationally, the proportion of patients waiting longer than two months to start cancer treatment following GP urgent referral has increased significantly over time. In November 2009, 13.8% of patients waited longer than two months to start treatment compared to 17.5% in November 2017. Since 2014, the cancer target has been missed for all but three months, and was last met in December 2015. In January 2017, over 20.3% of cancer patients waited longer than two months for treatment, representing 2,437 people.
2.8 Two month wait from a national screening service to a first treatment for cancer
In October 2017, 10.7% of patients waited longer than 62 days to start cancer treatment following referral from a national screening programme. This is only the second time that the target has been breached since 2009. However, the overall level of performance against the operational standard has generally been decreasing. In 2012, an average of 4.8% of patients breached the wait time target each month compared to an average of 8.0% in 2016.
A closer look at the two month GP urgent referral to first treatment for cancer target
With NHS performance against the two month GP referral to first treatment for cancer target floundering, we did some further analysis to explore the data.
Figure 3 separately ranks Trust performance data for 2010/11 and 2016/17. Trusts for which there was missing data were excluded. It is clear that a much larger proportion of Trusts missed the 15% target in 2016/17 compared to 2010/11. In 2010/11, 26 out of 144 Trusts missed the target but this increased to 76 out of 144 Trusts in 2016/17. This means that many more cancer patients are having to wait longer than two months to start treatment - this is deeply concerning as the more advanced a cancer is, the harder it is to treat.
Figure 3. Two month wait from GP urgent referral to a first treatment for cancer, ranked Trust performance for 2010/11 and 2016/17
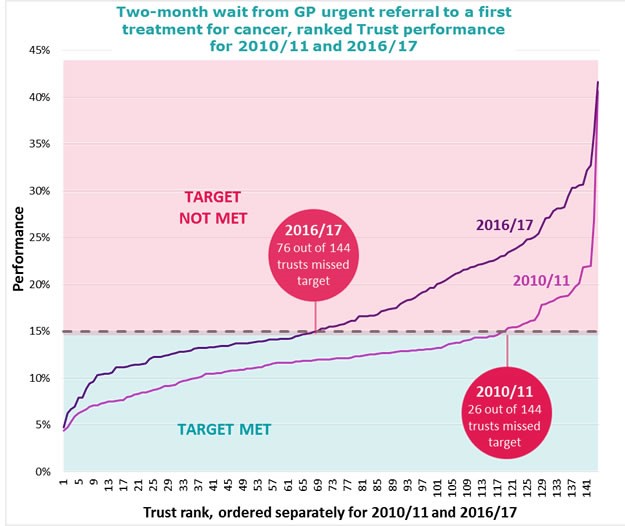
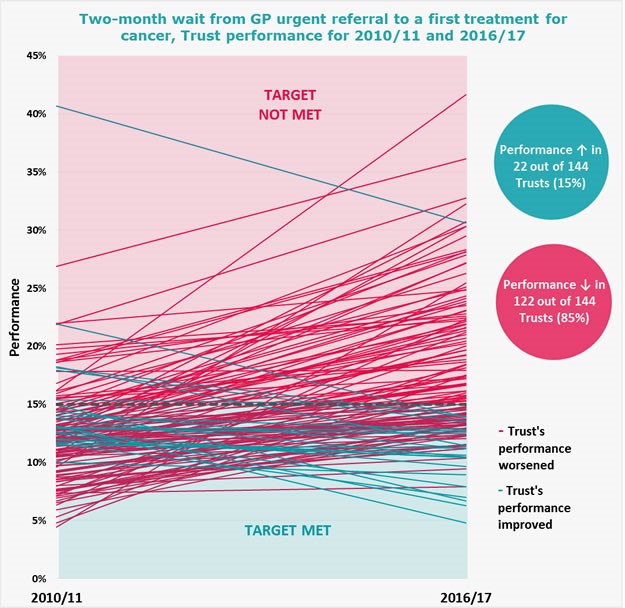
Figure 4 shows how individual Trust performance against the two month GP referral to first treatment for cancer target has changed over time. Each line represents a separate Trust. Performance worsened in 122 out of 144 Trusts between 2010/11 and 2016/17.
Figure 4. Two month wait from GP urgent referral to a first treatment for cancer, individual Trust performance for 2010/11 and 2016/17
Why is NHS performance against the two month GP referral to first treatment for cancer target worse than the other targets?
The headline NHS cancer target – that less than 15% of patients should wait longer than 62 days to start cancer treatment following urgent GP referral – has been breached in all but one month in the last three years.
But performance against the other targets has been relatively good. Almost all patients have their first consultant appointment within 14 days of GP urgent referral, and once a decision to treat has been made the vast majority of patients start their first treatment for cancer within 31 days.
Why is there such a disparity in NHS performance against these targets? There is currently a missing element in the cancer pathway which has no target – time to diagnosis. None of the current targets capture the time elapsed from GP urgent referral to the patient receiving a definitive diagnosis or cancer exclusion. Performance against the 62-day target may have worsened relative to the other targets as it measures the entire patient pathway from referral to treatment, meaning it is currently the only target which takes time to diagnosis into account.
NHS England’s introduction of the 28-day faster diagnosis standard will help to plug this gap in the patient pathway. It is also extremely important, as earlier diagnosis is a key determinant for cancer survival. Diagnosing more cancers earlier could be transformative in terms of reducing mortality and improving quality of life.
However, there is question of whether we should look to simplify the cancer waiting time targets, as recently occurred with the 18-week referral to treatment targets in 2015. The Independent Cancer Taskforce proposed that the two week urgent referral pathway was “no longer needed”. With eight cancer waiting time targets soon to become nine, this increasing number of targets may be adding unnecessary complexity to an already complex patient pathway. Focusing on the entire cancer pathway and its most important elements may help commissioners and providers to optimise patient outcomes.
Ensuring that cancer patients receive timely access to high-quality care, treatment and support should be a top priority for the NHS. But the introduction of a new waiting time target will not improve cancer outcomes on its own. It is also important to consider factors such as prevention, workforce, funding and research and innovation if we are to see lasting change.
