The Nuffield Trust has spent the last two years investigating acute medical services in smaller hospitals. In 2016/17 we surveyed 48 trusts – just over two-thirds of the trusts classified as smaller by Monitor. Our survey explored the pathways followed by patients needing acute medical care, such as someone with a respiratory illness or urinary infection.
Acute medical services face considerable challenges. At the heart of these is a rapidly changing profile of patients. They are older, more dependent and many have multiple conditions.
“90% of our take is elderly patients coming in with multiple comorbidities.”
Consultant physician, Site 12
They require a model of care that looks at their needs holistically, and supports continuity of care both within the hospital and between hospital and the community. Yet many patients experience precisely the opposite of this – fragmented and poorly coordinated care.
We found that service models are complex, and there is considerable variation in how different service components operate and who takes clinical responsibility for the patient and when. For example:
- ambulatory emergency care – variation in function, hours of operation and staffing
- acute medical unit – variation in referral criteria, size, length of stay and balance of clinical responsibilities.
Staffing concerns
But the most immediate and visible challenge to acute medical care is that of staffing. The findings from our survey showed significant gaps in medical staffing, with consultant and other vacancies difficult to recruit to. Nearly all sites we surveyed were having difficulty with junior medical staffing, with some sites believing that the gaps in junior doctor rotas are creating safety issues.
“There are three or four gaps in the middle grade rota. We have had nights where there is no middle grade in the hospital.”
Clinical director, acute medicine, Site 36
The problems with consultant staffing varied across sites. Some were totally reliant on locum acute physicians, while others had no vacant acute physician posts. Nearly all sites were challenged in constructing sustainable medical on-call rotas for out-of-hours cover.
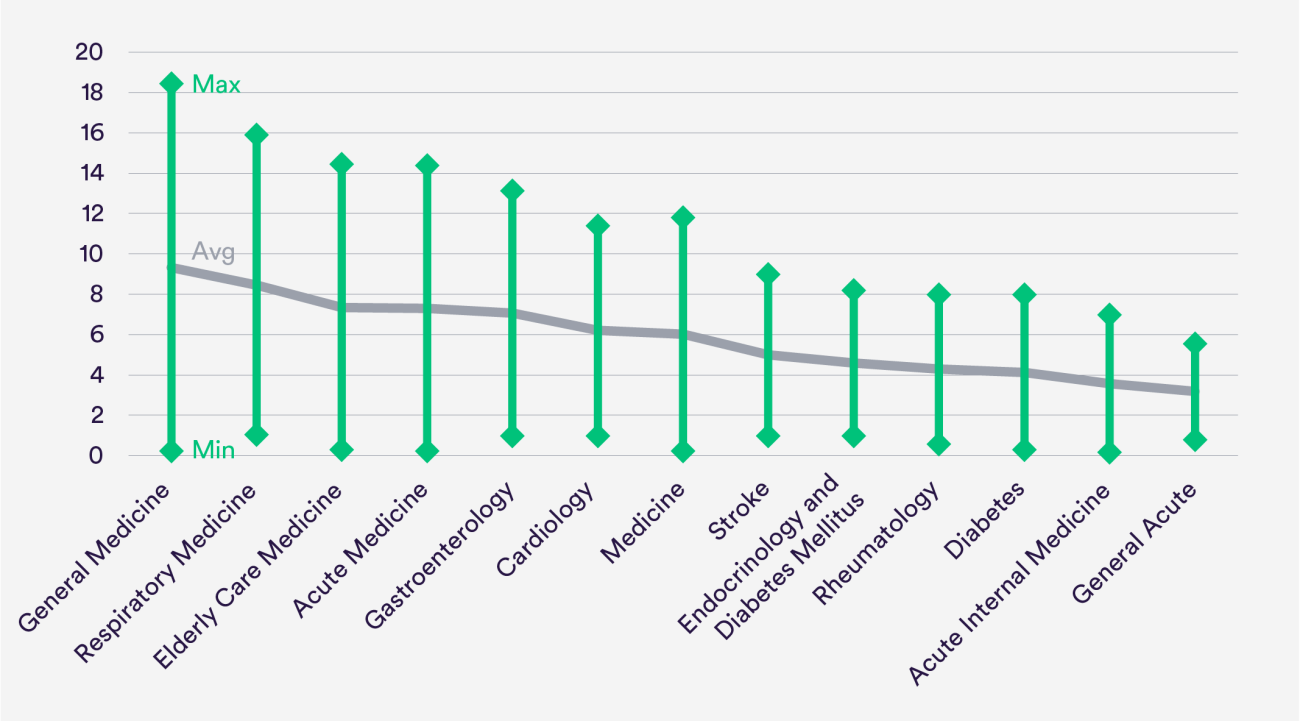
There was striking variation in consultant medical staffing across hospital sites.
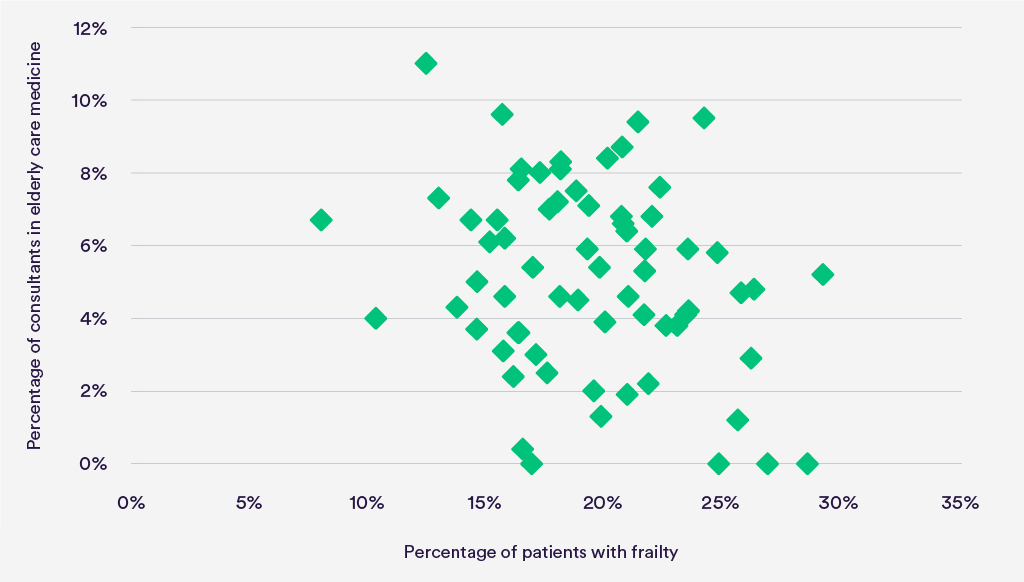
The variation could not be explained by variations in activity or case mix. A good example is geriatrics.
Why the variation?
A major constraint on staffing is the capacity to recruit. Many hospitals aspired to have more geriatricians and acute physicians but could not recruit them. In seven sites, more than half the acute physicians were locums.
“We’re never going to recruit six acute physicians, so we have to look at how the specialties can in-reach and deliver the acute medical take more than they are doing at the moment.”
Medical director, Site 6
But history clearly played a major part. Services had evolved over time on a ‘make-do-and-mend’ basis – building on what trusts had, both infrastructure and staffing. Services were in a state of considerable flux with much local improvisation. Every site but two had made changes to at least one aspect of acute medical services in the last year, and most were anticipating further change over the next year.
“They’re continuously designing and redesigning.”
Clinical director, Site 35
It was very striking, however, that consultant recruitment and service development tended to be specialty led, and rarely guided by an in-depth analysis of the patient case mix across a whole hospital. That is despite frequent acknowledgement by the respondents that hospitals should be adapting to this changing cadre of patients.
“So, if you’re in a gastro ward, you’ll be looked after by a gastro consultant: you may have a respiratory problem but you’ll be looked after by a gastro consultant. If you then move wards and end up on a cardiology ward, you’ll then be looked after by a cardiologist. So we’ve got care at the moment that is based on location of patient as opposed to patient need.”
Medical director, Site 6
Does this variation matter?
The extreme variability in the number of specialists suggests that some services are understaffed, potentially hindering delivery of good patient care, while others are potentially overstaffed, which may be indicative of over-servicing/waste.
Policy-makers also frequently encourage or mandate ideal models of care with little regard for the extreme variation in starting points. This may skew staffing decisions when hospitals are having difficulty recruiting enough staff to provide basic services. As a result, an organisation’s capacity to implement the new model of care may be adversely affected and the model’s ultimate impact diluted.
The profile of acute medical patients is changing rapidly, and staffing and financial constraints make it hard for services to adapt. But a shared ambition must be to achieve a closer alignment between the needs of patients and clinical skill mix for the benefit of both patients and staff. This needs to be undertaken at a whole hospital level.
*The results of the survey are now available as a slide deck resource.
This project, Models of Generalist and Specialist Care in Smaller Acute Hospitals: An Exploratory Study, was funded by the NIHR Health Services and Delivery Research programme – Reference number 14/195/02.
The views expressed in this article are those of the author and not necessarily those of the NHS, the NIHR or the Department of Health.
Suggested citation
Imison C (2018) "Caring for acute medical patients in smaller hospitals”, Nuffield Trust comment. https://www.nuffieldtrust.org.uk/news-item/caring-for-acute-medical-patients-in-smaller-hospitals