This week, the summary care record is back in the news. At the moment, if you become critically unwell and are taken unconscious to an A&E department, the doctors and nurses looking after you will typically have no idea of your past medical history, your allergies or what medicines you are taking. This is because they usually have no way of accessing your GP clinical record.
So, unless you happen to have old records in that hospital, the staff will have to treat you “blind.” Clearly this lack of information could be dangerous. Dangerous not only for unconscious patients but also for people who cannot communicate or cannot remember their medical details.
In Scotland, however, this hazard has been eliminated. Every single GP practice in Scotland now participates in the Emergency Care Summary (ECS) system. Launched in 2006, the national ECS provides out-of-hours clinicians with a core clinical summary, including basic details (name, address, date of birth etc.), emergency contact numbers, prescriptions, allergies and other adverse drug reactions.
This type of “data integration” across different parts of the health service is often sought but seldom achieved. So it’s highly notable that the ECS is now being used over 200,000 times a month across Scotland.
The ECS system works by extracting pre-determined details automatically twice a day from all GP electronic systems across the country, and making this information available through a secure website or “portal.”
Confidentiality
All patients are asked for their explicit permission to allow the emergency clinician to view their record. But in addition, a break-the-glass arrangement allows clinicians to access this information without consent if a participating patient is unconscious.
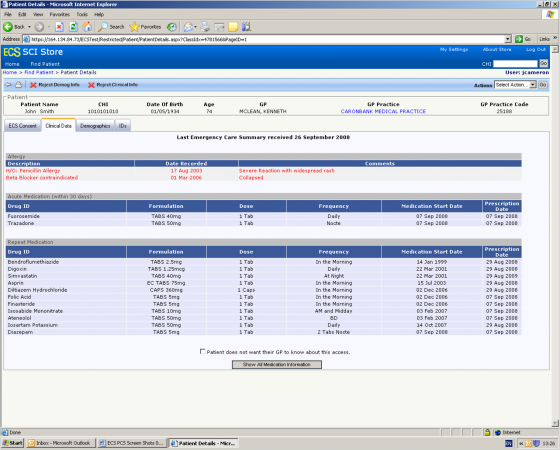
Figure 1 Scottish Emergency Care Summary (image and test data used courtesy of NSS Scotland)
So how come they have managed to achieve this in Scotland? One reason is that they began the project very carefully by commissioning the Scottish Consumer Council to conduct a detailed review of patient views. This consultation provided strong evidence that patients wanted the ECS, and it also set out a number of guiding principles for how the system should work. These included requiring explicit consent to view the record, insisting on a full audit trail, and rolling out the project incrementally across the country.
Future developments for the ECS include an expansion of the data to incorporate a palliative care summary, a record of patients’ wishes as well as ‘anticipatory care plans.’
At the moment, the only people who can “write” to the ECS are GPs and practice nurses. Out-of-hours practitioners can read the ECS but they cannot make changes to it. This current arrangement may not be ideal, but it reflects the pragmatic approach they have adopted towards data integration in Scotland.
Overall, this level of data integration across different parts of NHS Scotland is relatively modest when compared to fully integrated systems such as Kaiser’s HealthConnect™ or the VA’s VistA system in the United States. However, a forthcoming Nuffield Trust study (to be published in May 2011) on routes to integration found that less ambitious IT projects can be used to pave the way to closer integration over time.
Suggested citation
Lewis G (2011) ‘Data integration for emergency care: Scotland leads the way’. Nuffield Trust comment, 15 April 2011. https://www.nuffieldtrust.org.uk/news-item/data-integration-for-emergency-care-scotland-leads-the-way
