Next year (2014/15) is an important year – if all had gone to plan the structural current deficit would be eliminated and it would be the last year of austerity. It was also supposed to be the year in which almost all NHS trusts became foundation trusts (FT).
As it is, the Government is not expecting to close the current account deficit until 2017 and 100 NHS trusts are still not foundation trusts.
The combination of deteriorating finances and the new Care Quality Commission (CQC) inspection regime mean that very few will make it to FT status this side of the election.
The Health Select Committee is examining the NHS financial situation and our evidence summarises some of the recent analysis from the NHS Trust Development Authority, National Audit Office and Monitor examining the financial health of NHS providers. It does not paint a happy picture.
Foundation trust status matters to boards but has very little impact on patients. But the reasons why the pipeline has stalled highlight wider issues which will dominate the NHS over the next five years and for which at the moment there seems to be no convincing response.
As part of NHS England’s ‘Call to Action’, Monitor recently published a paper on the financial challenge with a slide pack from McKinsey. It’s a good paper but a very sobering read.
The first chart below shows Monitor’s analysis of the sources of potential NHS productivity gains and savings over the decade to 2021/22.
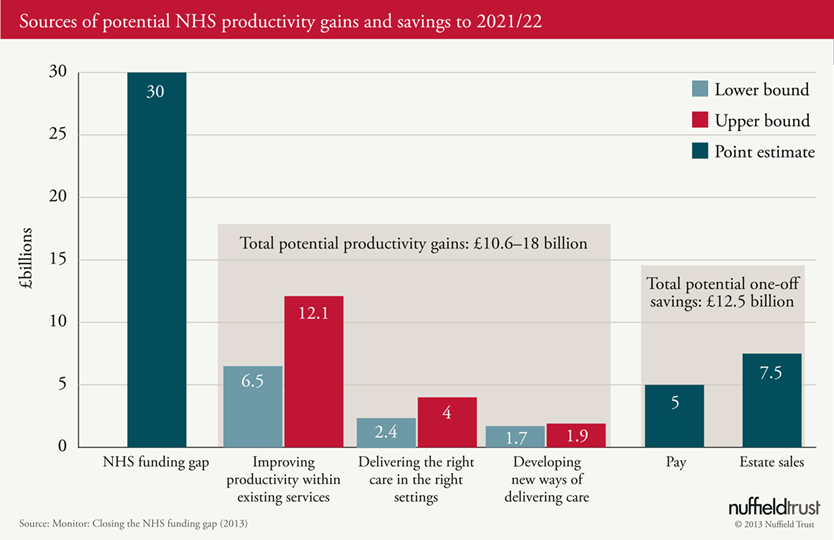
Three things stand out: first, that productivity gains from providers being more efficient at doing what you do now are the largest part of closing the gap (£6.5 – 12.1 billion); second, that Monitor isn’t banking on changing care patterns delivering large savings through this decade (this is probably a realistic assessment given the findings from current research in this area); and third, that pay restraint (which can’t go on forever) and asset sales (which are only one-off and very difficult to achieve) are essential to reaching the full £30 billion and even then they might not do it based on Monitor’s figures.
In essence, Monitor’s analysis confirms the findings of our earlier work: if NHS funding is held flat in real terms beyond 2015/16, productivity will not fill the gap and pay restraint is a short-term tactic which is likely to have run its course by the end of this parliament. Houston, we have a problem.
There is definitely scope for improved productivity and more appropriate care.
The Nuffield Trust, in partnership with the Health Foundation, recently published a study as part of the QualityWatch programme, which examined trends in emergency admissions and found that potentially avoidable admissions from ambulatory care sensitive conditions account for one in five of all emergency admissions and have been rising.
No doubt the NHS can improve productivity. Moreover, as a publicly-funded service there is an enduring responsibility to use public money well.
They increased by 48 per cent between 2001 and 2013 compared with a 34 per cent increase in all other emergency admission over the same 12 year period.
There are also a number of studies showing scope to reduce length of stay, improve first to follow-up ratios for outpatients and have better procurement. No doubt the NHS can improve productivity. Moreover, as a publicly-funded service there is an enduring responsibility to use public money well.
However, whilst analysis of the potential for improvement is important, it is becoming clear that despite pay restraint the NHS is already beginning to really struggle with the financial challenge and that this is most apparent in the acute sector and in the smaller acute hospitals (turnover of under £400 million).
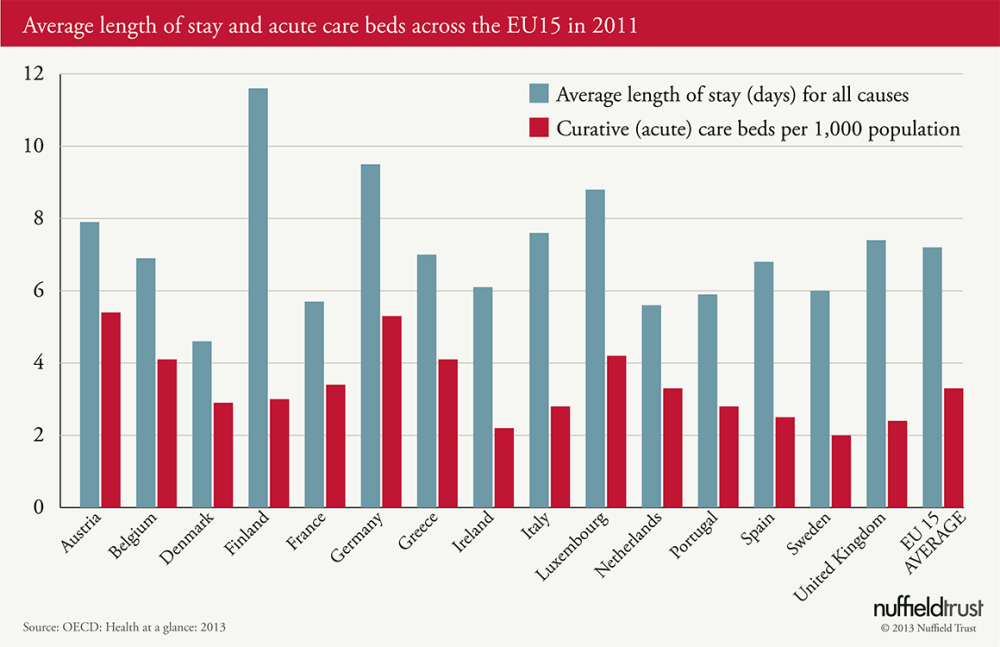
Looking at international comparisons, we also need to be realistic about how far we can push the acute sector without risking quality of care.
Comparing the UK to EU15 countries (see the second chart below), the UK does not have a large hospital sector (only two countries have fewer acute care beds per 1,000 population – Ireland and Sweden) and we run our service pretty hot with internationally high bed occupancy rates, although average length of stay is slightly above average.
Although the EU countries receiving support from the Troika are cutting health spending in real terms, most of the rest of Europe are still increasing their spending on health in real terms.
We are trying to do something pretty unprecedented: driving really deep productivity gains to make us world leading on acute sector efficiency; raising quality to make us world leading; and changing the patterns of care to meet long-term conditions/frail elderly better and make us a world exemplar. And they all have to come right because we have no additional cash.
It is good to be ambitious and to change the paradigm would be a triumph which would be the envy of the developed world but banking on it looks very high risk – we need a plan B urgently.
