Many GPs are on their knees and exploring options to save their practices, and the most frequently cited solution by practices and commissioners alike seems to be collaboration – joining together into large-scale groups of practices.
A few weeks ago the Nuffield Trust hosted a conference, Large scale general practice: can we rise to the challenge?, to weigh up the benefits and challenges of working at scale.
The day was full of great speakers and discussions, but an early reflection from an audience member really set the tone. The comment came from a young GP partner who described how the levels of morale and funding in practices were currently crashing and how he looked forward to the benefits of large-scale working turning things around. He likened the trajectory to a J-curve, looking something like this:
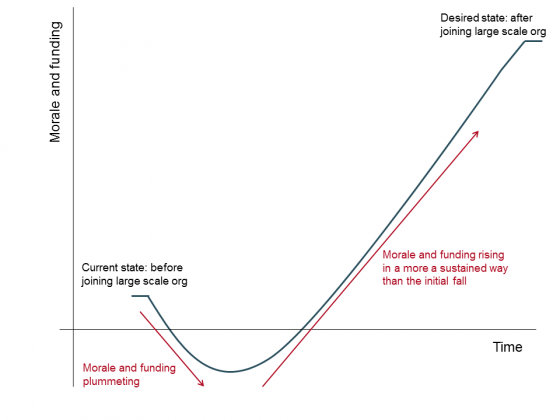
Having just completed a 15-month study where we interviewed over 100 staff in four large-scale general practice organisations – the results of which will be published next week – this comment really resonated with me. While the GP was right to be optimistic in some ways – there are definite benefits to working at scale – one message from our research was clear: working at scale takes significant effort, energy and financial investment from both leaders and members.
Making it work is not going to be easy. This conference was therefore an important chance for GPs to come together to discuss the benefits and the pitfalls; to share tips and tricks from their own experiences.
The combined experience in the room made for some interesting discussions, insights and lessons.
Why should GP organisations work at scale?
Everyone had a good reason to collaborate. In a presentation drawing on our upcoming research, Rebecca Rosen told us that the key benefits of scale were to prevent practices from closing by sharing income, staff and administrative burdens. She also described how most staff enjoyed working in large-scale organisations, had better training and development opportunities, and felt a sense of community that made day-to-day challenges easier to deal with.
Helen Parker of Midlands Health Network, one of New Zealand’s four largest GP organisations, explained how a network approach provides numerous advantages, including the chance to share data to monitor local trends and decrease variation across practices. She also explained how central managers reduce burdensome admin and improve the working lives of practice staff, to “take the pain away from practices”.
Arvind Madan of NHS England agreed. His experiences working in Tower Hamlets proved to him that single-handed practices were particularly well-placed to benefit from centralised administrative and peer support.
So what’s the down side?
But it's clear the challenges associated with realising these benefits are huge. Leadership is hard. Rebecca highlighted trends in our research that suggested 'heroic' leadership from senior staff, including working very long hours, was necessary.
Mark Spencer, Co-Chair of Collaborate, a primary care leadership-focused initiative, told us that clinical leaders played an essential role in engaging staff, but were also expected to know how to chair a meeting, set governance requirements and interact with the public – all very daunting tasks if your previous roles haven't given you the necessary training or experience in these areas.
Furthermore, paying for central management and administrative teams is hard and requires upfront investment. These functions are often funded by top-slicing community contracts or through financial contributions from member practices when the organisation is formed. Another option is national funding – which Arvind outlined as available for both individual practices and large-scale organisations. But winning money is a competitive business, and it can be very difficult to predict the costs to be factored into bids. It is similarly challenging to know with certainty whether initiatives that are meant to create efficiencies will actually do so.
Setting up these models, and making them work, is no picnic. Yet, in spite of the challenges, we know from our research that there are gains to be made that might just make it worth the hard graft. Indeed, the general sense among conference delegates was that they were up for the challenge.
Here are seven key tips to emerge from speakers on the day:
Top tips on how to work at scale
-
Maureen Baker: Make sure that GPs who have the appetite for scaling up are involved – act as leaders and maintain the grassroots movement. This means taking part in the STP process as well.
-
Mark Spencer: Invest heavily in leadership training and connecting leaders across the country to share experiences through the Collaborate movement.
-
Sharon Lamb drew on her personal experiences of 10 years as a partner at Capsticks law firm and suggested that organisations must be prepared for governance structures to change rapidly as the services offered and business models change. And as organisations grow, member practices should anticipate fallouts between leaders and expansion of teams to bring in areas of expertise valuable to the organisation – it’s all part of development.
-
Helen Parker: Maintain face-to-face contact; being familiar with all GPs helps to spot problems early and deal with them. However, Helen argued the benefits of scale – namely, the abilities to fund a large central team to facilitate change in practices, collect data rigorously, and monitor trends (allowing for a population health focus) – are best realised with large registered lists of 200,000 or more patients.
-
James Kingsland: Following social network size theory, James argued for keeping the registered patient population under 50,000 and staff teams to 150 people or fewer to keep transaction costs low and ensure that teams know each other (and their patients – to increase personlisation in general practice).
-
Arvind Madan said that large-scale organisations facing recruitment challenges should think about offering portfolio careers, local practice resilience teams and flexible career structures – some of which can be funded by local CCGs.
-
Southwark Clinical Commissioning Group: Pitch extended access initiatives to patients as extensions to their familiar practice: patients feel more comfortable with their records being shared and are more likely to use them.
Many of these tips reflect the lessons that arose from our research examining large-scale general practice organisations over the last year or so. Our report Is bigger better? Lessons for large-scale general practice will be published next week, and provides detailed evidence-based lessons for emerging organisations.
