Key findings
The NHS clinical support workforce are frontline staff who – while typically not registered professionals – deliver the bulk of hands-on care. They are particularly important to mental health services where there is an ambition to, for example, provide high-quality mental health services to an additional two million people by 2023/24 1. This report explores the roles, responsibilities and diversity of mental health clinical support staff. Our aim is to draw out the number and distribution of this workforce and issues around their recruitment, career progression and retention.
About the mental health clinical support workforce
The clinical support staff in mental health services make up a large proportion of the overall NHS workforce. There are nearly 340,000 full-time equivalent clinical support staff across all NHS hospital and community health settings, which is larger than the nursing and midwifery workforce. Around one in eight of these (just over 41,000) work in mental health services. They account for more than a third of clinical staff working in mental health.
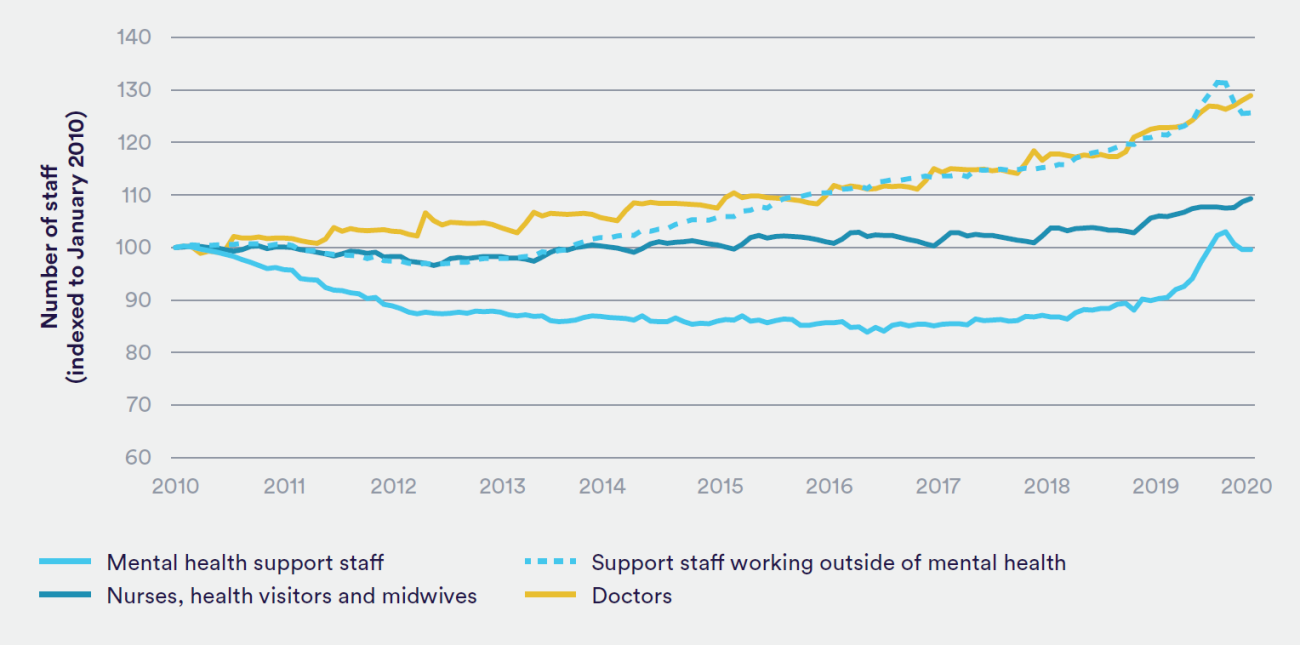
There had been a decrease in the number of mental health clinical support staff over the previous decade. While there was a significant increase between January and July 2020, it then started to fall; this fall could be partly due to staff in short-term positions recruited during the early stages of the Covid-19 pandemic reaching the end of their contracts. A similar pattern was seen for clinical support staff in other hospital and community services during those months of 2020; however, unlike the mental health support workforce, before 2020 there was fairly consistent growth in this group (see Figure 1). The precise reasons for the fall in the number of mental health clinical support staff during the 2010s are unclear, although we previously highlighted a similar finding for the number of mental health nurses during the decade 2. There is an expectation that the mental health clinical support workforce will grow with, for example, the NHS Mental Health Implementation Plan 2019/20 – 2023/24 suggesting an indicative need for more than 6,000 more clinical support staff by 2023/24 3
Mental health clinical support work encompasses a variety of different roles and staff can work with a huge range of people and services and in a wide variety of settings. In fact, we found that within the electronic staff records of mental health clinical support staff there are some 96 unique job titles. While there is certainly an array of different roles and therefore a high number of job titles is not unexpected, some of these appear to describe the same role. A lack of clarity and consistency in role titles is a longstanding issue but also potentially problematic, given titles can help indicate to both fellow workers and patients where responsibilities lie.
There is no consensus on role hierarchy across the mental health clinical support workforce or the categories of similar roles. However, for the purpose of interpreting the findings presented in this report, it is worth considering the workforce as three somewhat broad categories:
- health care assistants and those in similar positions who work within defined parameteres and boundaries, typically under the supervision of a registered professional
- those in 'professional' roles, which typically require advanced or further education - some, such as nursing associates, are registered
- those in training posts, such as trainee psychological wellbeing practitioners, who are employed as clincial support workers while seeking to become part of the qualified workforce.
Roles, requirements and responsibilities
There are published standards for some – but not all – health care support workers and, in reality, there appears to be substantial variation in the stated responsibilities of individual support workers. There seems to be some similarities in the responsibilities of mental health support workers, which typically span clinical duties, information responsibilities and ensuring a safe environment for patients. However, the degree to which these staff are expected to supervise other staff appears to be inconsistent, even for those on the same pay level (banding). The Code of Conduct for health care support workers in England4 outlines their key responsibilities but it is a voluntary set of standards, which only formally applies to those who report to a registered nurse or midwife in the NHS.
While there is currently no universal, mandatory standard for the education and training of clinical support workers in England, many NHS trusts have adopted the voluntary Care Certificate, which has been designed primarily for those new to care, to reduce inconsistencies in their training. The situation in the other nations of the UK is different. Northern Ireland and Scotland have gone further to introduce mandatory induction standards and a Code of Conduct for health care support workers5.
Scotland and Wales have also introduced a Code of Practice for employers67. In addition, Wales introduced a Skills and Career Development Framework for all support workers in 20168 . Meanwhile, the Francis Inquiry report recommended the compulsory registration of health care assistants9– an idea supported by support workers at the time10 – however, this is largely still not the case across Europe.
There is marked, unexplained variation in the experience, knowledge, qualifications, skills and values that NHS organisations seek when employing mental health clinical support staff. These requirements often also differ compared with what is indicated on the NHS Careers website. For example, from the mental health support worker job adverts we reviewed, qualifications listed as essential ranged from basic literacy and numeracy to a National Vocational Qualification (NVQ) level 311 in a relevant subject. While some variation might be reasonable given the different requirements of individual roles across specific settings, this warrants further investigation.
Clinical support staff are some of the lowest paid in the NHS. Staff in NHS hospital and community settings are typically employed on the Agenda for Change pay framework, which covers around 88% of NHS staff in England. The support staff we focus on in this report are paid between band 2, which starts at £18,005 (in 2020/21), and band 4, which goes up to £24,157.12 The mean pay of clinical support staff increased by 13% over the nine-year period between 2011 and 2020 – broadly in line with inflation – with the minimum salary increasing by almost a third (31%). However, there appears to be unexplained variation in the level of pay for similar roles. Previous research – backed up by our own review of job adverts for this report – suggested that mental health support worker roles were particularly varied in terms of banding (that is, pay level), even after excluding ‘senior’, ‘specialist’ or ‘advanced’ positions13.
Participation
Mental health clinical support workers typically work full time. Within mental health services, clinical support staff are contracted to work, on average, an equivalent of four-and-a-half days a week – representing 0.91 full-time equivalents. This is higher than for support staff in other hospital and community services (0.86) and for nurses and midwives (0.89).
There is a striking difference between the stated intention to provide flexibility to NHS workers and the reality of flexibility advertised for mental health support roles. For example, the NHS’s People Plan 2020/21 outlined the benefits of flexible working for NHS staff, noting that it is good practice to offer the option of flexible working from day one14. However, at least half of the job adverts for mental health support workers we analysed stated that flexibility was expected from the successful candidate rather than offering a flexible working pattern, with many setting out expectations for them to work unsociable hours over a sevenday week. While it is important that some services can provide 24/7 care, this contrasts with the stated intentions around flexibility. The proportion of staff reporting being satisfied with opportunities for flexible working patterns is lower for clinical support staff working in mental health (56%) and other settings (53%) compared with that of all mental health staff (62%). From September 2021, NHS staff will have the contractual right to request flexible working from day one; it is important that this benefit is applied consistently15.
There will always be times when staff become unwell and are unable to attend work. However, the reported levels of sickness absence across the clinical support workforce in hospital and community services16 are high (6%) compared with other staff groups such as nurses (5%). While it is important to note that data on sickness absence need to be treated with caution due, for example, to different ways in which sickness is reported across staff groups, the relatively high rates among clinical support workers suggest that more could be done to address workplace issues that can lead to, cause and sustain absence.
Retaining existing staff is important to the NHS, not only to ensure there are sufficient numbers of staff but also to retain the skills that staff have gained during their service. There is little information on the lengths of career of mental health clinical support staff. However, across all clinical support staff, ‘health, adult dependants or child dependants’ accounted for a greater proportion of voluntary resignations (13%) than for all staff (8%). Dismissal accounted for 5% of staff leaving their clinical support job, compared with 2% of all staff.
Supervision, training and career progression
The role of the first line manager is critical to ensuring that clinical support workers are appropriately valued, supervised and held to account17. Historically, there have been issues concerning inadequate supervision of support workers18. Of those responding to the NHS Staff Survey in 2019, the proportion of mental health support staff who were satisfied with the support they received from their immediate manager (75%) was similar to that for all staff in mental health trusts (76%), but higher than that for support staff working in other settings (70%).
One of the stated intentions is to support the career progression of NHS workers. The People Plan 2020/21 committed to a ‘continued focus on upskilling – developing skills and expanding capabilities – to … support career progression’19. However, the development of many clinical support staff groups does not appear to be a priority. There have been longstanding issues around fragmented and variable educational opportunities for clinical support staff20. Health care assistants, for example, are likely to spend the most time out of all mental health roles providing direct care to patients, but are likely to receive the least training and supervision21.
Efforts have been made to develop a training and development framework for unregistered workers, namely the introduction of the Talent for Care programme in 2014 and the subsequent report The Talent for Care, which sets out the Talent for Care national strategic framework22. This programme aims to support NHS organisations with their workforce supply through, for example, work experience, apprenticeships and access to higher education and the registered professions. It also seeks to aid the sharing of best practice. Although the Talent for Care report presents a breadth of evidence of work being done, in particular for developing apprenticeship strategies, work still remains to highlight what can be done for the mental health workforce specifically.
While many job adverts we reviewed referred to ‘excellent training facilities’ and ‘a range of development opportunities’, the specific job descriptions rarely went beyond ‘training appropriate to the role’, including induction, mandatory minimum training and the supervision process supporting development. In some cases, there was no mention of training in the adverts. These training issues are important; a ‘lack of education, training and development opportunities contributes to poor quality care’23.
Patterns of actual progression require further investigation. Analysing experimental data provided by NHS Digital, we found that in hospital and community services other than mental health, the probability of progressing from the different clinical support workforce pay bands is consistent – at around 9% over the course of a year. However, in mental health services, the probabilities vary: around one in five members of staff on band 2 as at June 2019, who stayed in the NHS, had progressed to band 3 (or above) by the following year; while only one in 16 members of staff on band 3 who remained in the NHS moved onto a higher band. This may, however, reflect the number of training roles in mental health.
For those not in training posts, there is limited movement between roles. More than nine in 10 (93%) of those who were mental health support workers or health care assistants in June 2019 and who were employed in the NHS the following year remained in the same role, with just 1% moving into trainee nursing associate roles. It is positive that there are now some complete pathways into professions through apprenticeships, such as from health care assistant to nursing associate, to nurse degree apprentice and, even then, to advanced clinical practitioner24. However, the apprenticeship scheme is not specifically designed for the NHS and, while some changes have been made to incentivise NHS trusts to provide certain courses, there remain challenges (Beech and others, 2019). In particular, while recent funding will incentivise the provision of nurse degree apprenticeships, a question remains as to how much of employers’ apprenticeship levy will be invested in the clinical support workforce and indeed whether other continuing professional development efforts and funding will be directed at this staff group.
Equality and diversity
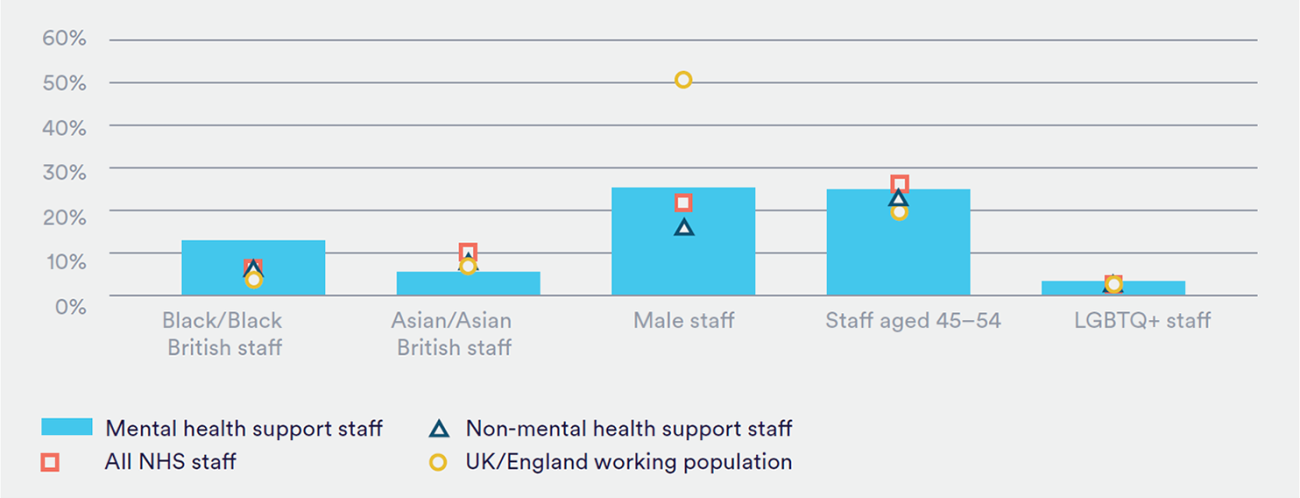
The current demographics of the mental health support workforce are quite distinct from the NHS as a whole. Compared with all NHS staff, the workforce have a greater number of both Black/Black British staff and male staff (see Figure 2). Little is known about some other protected characteristics such as pregnancy, maternity and gender reassignment status or other demographic factors such as socioeconomic status. Promoting a more diverse workforce can help ensure a sufficient and sustainable supply of clinical support staff. A diverse workforce also means it is likely to be representative of communities that are ‘particularly disadvantaged within the present system’25.
The picture on ethnicity and gender pay gaps is complex. There were no obvious differences in career progression – that is, the probability of moving up pay bands – between different ethnicities in our analysis of experimental data. However, previous novel analysis has suggested that across staff working in a support role to doctors, nurses and midwives (in mental health and other settings), there is an ethnicity pay gap in favour of white staff (Appleby and others, forthcoming). Unusually, the gender pay gap in support roles is apparently in favour of women26.