NHS finances
Current annual health spending is £124 billion in England or £149 billion across the UK.[i]
The NHS has been under serious financial strain recently across the UK. In England, it has been receiving funding increases of less than 1 per cent a year, compared to around 4 per cent on average over its history.[ii] Spending has also been roughly flat in Scotland, Wales and Northern Ireland. English NHS trusts have run up repeated overspends in the last few years, most recently £791 million.[iii]
The financial situation plays into pressure on targets as the availability of beds and staff becomes increasingly stretched. For example, the four-hour A&E target was missed in all four countries during the 2016/17 financial year.
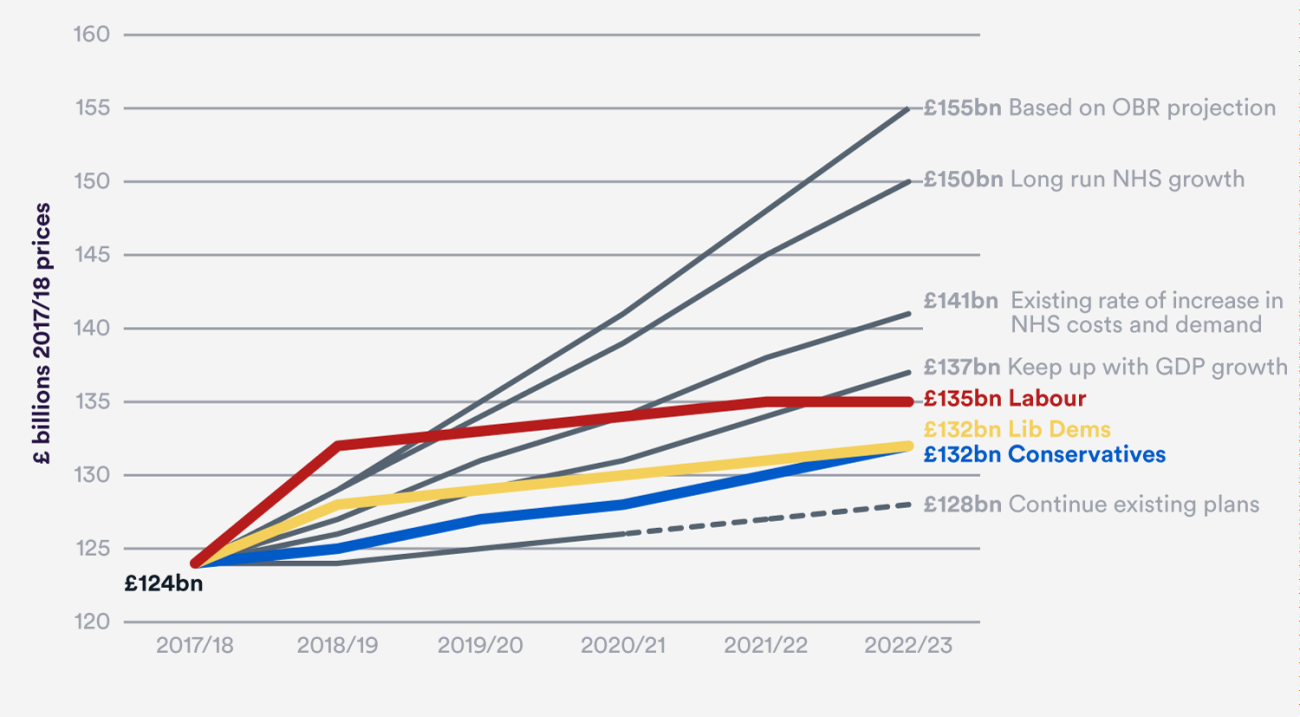
We looked at four measurements of how much the Health Service will need by the end of this Parliament. Although all parties’ manifestos pledged significant increases, none would even keep NHS spending rising in line with the wider economy – the minimum scenario we considered. All fall far short of keeping up with costs and demand.[iv]
Without more funding, pressure on services will continue and expectations of what the NHS can deliver will need to be kept realistic. New targets or ambitions are unlikely to be achieved.
Social care
Health care is provided free to everyone by the NHS in England and Wales. But council-funded social care for older people, helping people suffering from frailty and dementia with everyday activities like washing and dressing, is available only to those with the least assets and most severe needs. This is a longstanding anomaly.
The number of people aged over 85 is set to rise by 0.5 million (33 per cent) between 2014 and 2024.[v] Yet the Association of Directors of Adult Social Services estimates that £1.6 billion has been cut from local authorities’ adult social care budget since 2010.[vi] The Nuffield Trust and King’s Fund calculated in our 2016 joint report on social care funding that cuts to local authority budgets mean that 26 per cent (250,000) fewer people are now receiving care packages from their local council than five years earlier.[vii] A funding gap of £2.1 billion is set to emerge by 2019/20.
The current system is also marked by unfairness, with one in 10 people unlucky enough to have serious needs paying more than £100,000.[viii]
We have called on the Government to devise a long-term, fair and sustainable solution to the problem of how we fund the care almost all of us will need in our old age. This could include the proposal for a cap on individual payments, already passed into law and pledged by all parties, or proposals to raise the amount of assets people can have and still receive free care. However, fully addressing the issue of unfairness may require an insurance system alongside this. So far, voluntary private insurance has failed to take hold, so the Government should continue to consider a social insurance system where costs are pooled across everybody, as exists in Japan.
Workforce
The NHS across the UK employs 1.7 million staff, making it our largest employer. But there are currently serious shortages. The National Audit Office found 50,000 vacancies among all clinical staff in 2014. The Royal College of Nursing has found that one in nine nursing posts, or about 40,000, are vacant in England alone.[ix] This is a particular concern because ratios of nurses to patients are important for safety. The Department of Health believes that if Brexit shuts out future nursing migration, it could cause an additional shortage of 20,000 nurses by 2025/26.[x] Largely as a result, hospitals in England spent £2.9 billion on agency staff last year, typically at higher costs.[xi]
There are particular problems with GPs and district nurses at a time when the NHS is trying to do more outside hospital. Recent data from 866 practices shows 430 GP posts vacant – one vacancy for every two practices.[xii] The number of NHS district nurses has fallen by more than half since 2010.[xiii] Part of this is due to more private companies and charities taking on work, but experts believe there is also an underlying drop in numbers.
There are also growing difficulties in medical recruitment and retention. Hospitals are struggling to fill consultant posts in some specialties and locations, with a knock-on effect where junior doctors are taken out of hospitals if staffing shortages mean their training cannot be safely supervised. Furthermore the proportion of junior doctors entering specialist training to become consultants has fallen dramatically, possibly as a result of the protracted contract dispute. Last year, only 50 per cent of trainee doctors progressed directly to work as NHS specialists.[xiv]
Brexit
Although the £350 million extra per week that the Leave campaign implied would be available to the NHS is a myth, the net £7.1 billion we do give the EU each year could free up more than £100 million more a week for the NHS.[xv] However, the OBR estimate that a short-term slowdown associated with Brexit will take £15.2 billion out of Treasury funding by 2020.[xvi]
In the year before Brexit, one in three new nurses came from the European Economic Area.[xvii] Figures show a dramatic fall of 95 per cent in nursing migration from Europe since Brexit.[xviii] If this continues, it will add to an already serious shortage. In social care, we calculate that if unskilled EU migration is shut off there could be a shortage of 70,000 workers by 2025.[xix]
Currently, the NHS can buy medicines from across the EU as all countries are regulated by the European Medicines Agency (EMA). This helps avert shortages and makes us part of a priority market for cutting-edge drugs. After Brexit the UK should either remain subject to the EMA, or come to an arrangement to recognise its rulings so that these benefits continue.
The EU’s S1 scheme allows UK pensioners to receive care abroad: we estimate that if they had to return, their care could cost £500 million more to provide within the UK (the £1 billion cost of that care minus the amount already spent on their care through the S1 scheme).
However, there are also EU regulations some in the NHS would like to change, like the Working Time Directive which limits the hours doctors work, and the requirement to put contracts out to competitive tender. Our ongoing agreement with the EU will decide whether these still apply, and it will be important to remember the impact on the NHS.
Public health
Improving public health is one of the only ways to alleviate pressure on the NHS in the long term, while improving health lifespans. Yet obesity and excess weight have slowly risen to 63 per cent of adults in England, one of the highest rates in Europe.[xx] Measures of the health of children, including obesity and mortality, again lag behind many similar countries and are an area of particular concern. Issues of public mental health are only beginning to be addressed, even as the rate of under-18s presenting at A&E with a psychiatric condition has doubled between 2010 and 2015.[xxi]
Improving the health of the general public, through regulation, financial measures and the work of all public services including the NHS must be an urgent priority for this Parliament, and we call for bold action.
Moving care out of hospital
Removing the need for many patients to be treated in hospital is the holy grail of health policy. There is a hope that if more people receive their treatment from GPs or nurses in the community, or even in their own homes, it will both cost less and be less inconvenient and disruptive for the patient. This vision underlies NHS England’s Five Year Forward View, and has also been adopted by the Welsh and Scottish NHS. However, so far it has not happened: emergency admissions to hospital have risen by 14 per cent since 2008/09.
Our research has shown that while schemes to shift care out of hospital often are better for patients, the assumption they will save money is not always right. Of the 27 initiatives we examined (which included schemes such as hospital consultants holding clinics in the community and extending GP opening hours), only seven clearly saved money. Nine had mixed evidence on whether they actually saved money, while six were found to potentially cost more.[xxii]
These findings have particular implications for the new ‘Sustainability and Transformation Plans’ (STPs) which now cover the whole of England, all of which contain several of these methods of managing patient demand. Scottish Integration Authorities, and Integrated Plans in Wales, are pursuing similar projects. We firmly believe that these more joined-up ways of planning are the right thing to do, but there is a need to be realistic about how much money they will save.
References
[i] What is the NHS budget?, Full Fact
[ii] The Autumn Statement 2016 - Joint statement by The King’s Fund, Nuffield Trust and The Health Foundation on health and social care, The King's Fund
[iii] Quarterly performance of the NHS provider sector: quarter 4 2016/17, NHS improvement
[iv] Political party manifesto pledges, Nuffield Trust
[v] Shifting the balance of care: Great expectations, Nuffield Trust
[vi] Social care funding, Full Fact
[vii] Social care for older people: home truths, Nuffield Trust
[viii] Social care – a step forwards or a step backwards?, Institute for Fiscal Studies
[ix] Safe and Effective Staffing: the Real Picture, Royal College of Nursing
[x] Getting a Brexit deal that works for the NHS, Nuffield Trust
[xi] Performance of the NHS Provider Sector year ended 31 March 2017, NHS Improvement
[xii] General and Personal Medical Services in England 2006 – 2016, NHS Digital
[xiii] Understanding quality in district nursing services, The King's Fund
[xiv] Half of foundation trainees now choose not to progress straight to specialty training, BMJ Careers
[xv] Letter from Sir Andrew Dilnot to Norman Lamb MP: UK contributions to the European Union, UK Statistics Authority
[xvi] Economic and fiscal outlook – November 2016, Office for Budget Responsibility
[xvii] The UK nursing labour market review 2016, Royal College of Nursing
[xviii] New data show 96% drop in nurses from EU since July last year, The Health Foundation
[xix] Getting a Brexit deal that works for the NHS, Nuffield Trust
[xx] Briefing paper: Obesity Statistics, House of Commons Library
[xxi] Building communities with resilient children at their hearts, Nuffield Trust
[xxii] Shifting the balance of care: Great expectations, Nuffield Trust