As the longest election campaign in living memory moves into its closing stages, the main political parties are working harder than ever to emphasise the differences between themselves and their competitors. This is especially noticeable when it comes to the NHS, which has been one of the key battlegrounds of this election. But does the choice of political party really make that much of a difference to health system performance?
Fortunately, we have a natural experiment with which to test this hypothesis. The UK has operated four health systems since devolution in the late 1990s and many different policy choices have since been made. Different political parties currently control each UK health system, meaning that any differences between the performances of the health systems can be highlighted as having political significance. But do the choices made by politicians result in demonstrable differences in outcomes?
What do we know?
How have political leaders tried to make big changes to the UK health systems?
Over the past decade, some notable policy differences between the countries have included England’s pursuit of aggressive performance management and internal markets, and Wales’ emphasis on prevention and public health. In Scotland there has been noticeably less appetite for the organisational changes seen south of the border, and both devolution in 1999 and the more recent independence referendum saw prompted strong rhetoric against ‘privatisation’.
No one would doubt that political leaders have substantial influence on how their health systems operate. Indeed, in the course of this parliament we have dramatic changes in the way the health system is organised in England. The question is to what extent do these changes affect the performance of their health system?
How would we know if it made a difference?
While the changes made by politicians are easy to see, accurately comparing the performance of the systems is not as straightforward as it might appear. To do it robustly would require accounting for differences in outcomes related to differences in the population, for example, age, deprivation and rurality. The published data rarely allow for such adjustments. In fact, just obtaining any comparable data is a struggle. Given the many things that the four countries of the UK share in common and the importance of data to modern health care, it is surprising that one area where there is increasing divergence is the information systems.
Several comparative studies of the UK health systems have been published in recent years – fromourselves, fromThe King’s Fund and from the National Audit Office. All of them encountered difficulties in finding comparable data, and it seems that the number of comparable measures is decreasing over time. Here we look at just two specific examples where broadly comparable data are available.
A specific example: Time spent in A&E
The speed with which people move through A&E is regarded as a sentinel marker of the health care system across the UK. All four nations measure the percentage of patients spending less than four hours from arrival at A&E, and all currently work towards a target of 95%.
Yet, even this apparently simple measure is potentially misleading. England has a very different mix of what are classed as ‘A&E units’ than the other countries, with more minor units. These treat less serious cases and find it much easier to meet the four hour target. If we take only the major units for each country (see the figure below), we see that England is the only country ever to reach 95%, and it generally has higher levels of achievement than the other countries. This is often attributed to the political choice to prioritise achievement of the four hour target in England, and the ‘targets and terror’ regime used to implement it.
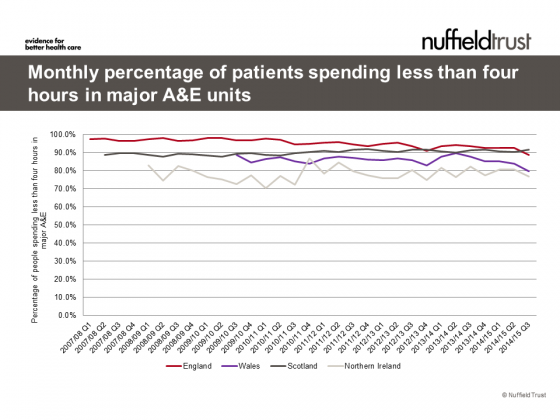
Sources: England , Wales , Scotland, N. Ireland
However the story is not that simple. The four hour target was maintained in England despite a change of government that saw many other targets removed. More recently, both England and Wales have seen deterioration, while Scotland continued a slow but steady upward trend.
And importantly, after 15 years of various differing health policy choices, the range of performance across the countries is just one person in ten spending more than four hours in A&E.
While time spent in A&E is a measure of access to care, there are many other ways in which people access healthcare. A broadly comparable measure of ambulance performance shows decline in every country since spring of 2014. We do not have reliable, comparable information on the ease of making a GP appointment or waiting for planned hospital treatment.
Another specific example: Cancer survival
Access to care is essentially a process measure. The link between national health polices and actual health outcomes is even more challenging to unravel. For example, looking at the most basic indicator of a successful health service – survival – differences between areas are influenced by a whole range of factors outside the health system and can take decades to have an effect.
One area where there is common information is in some of the national clinical audits. These can be used to cast some light on limited sets out outcomes. A study of cancer survival reported improved survival across England, Wales and Northern Ireland in breast, ovarian, lung and colorectal cancer. Improvements in one- and five-year cancer survival for Scotland are evident from other sources , but a different methodology means these are not directly comparable to England, Wales and Northern Ireland and are shown in the figure below for reference only.
While there are differences between the countries they are relatively small and often not statistically significant. With the exception of ovarian cancer in Northern Ireland, all survival rates follow the same trend and appear to be converging.
Five year cancer survival (with approximate 95% confidence intervals for Wales and Northern Ireland)
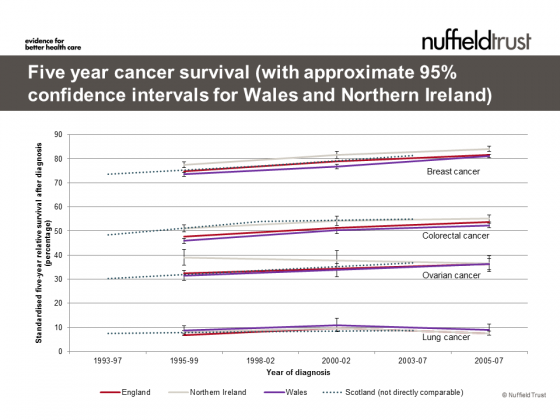
^England, Wales and Northern Ireland includes fallopian tube and adnexa cancers; * England, Wales and Northern Ireland excludes trachea cancers. Sources: Coleman (2010) and ISD (2010)
Are we expecting too much?
While all politicians want to improve health outcomes, the tools available to them to do this are indirect. Instruments such as service specification, structural reform, regulation and standards, and competition are all hotly debated in their ability to enhance outcomes.
Of all aspects under political control, perhaps health service funding is the most influential – something that will be explored in more detail in a future blog. All four UK countries have struggled in recent years with how to reconcile falling public expenditure with rising demand for health and social care. It can be argued that it is these funding decisions that have had the most substantial difference to health system performance.
Fact or fiction?
The data available to make comparisons between the four health systems in the UK are limited and becoming fewer, meaning our understanding of the comparative performance is cloudy. For the specific areas we have looked at we can see some small differences between countries but the scale of these differences seem rather marginal compared to the ambition in the political rhetoric.
While politicians can have some effects on culture, structure, expectations and policy levers, the effect of these is often less powerful than they expect or take much longer to have an impact than they think. They key difference they can make is often around the level and prioritisation of funding, but even here the impact may take time to be felt and the level of difference that can be made may be small.
Suggested citation
Blunt I (2015) ‘Fact or fiction? Politicians make a difference to health system performance’. Nuffield Trust comment, 2 April 2015. https://www.nuffieldtrust.org.uk/news-item/fact-or-fiction-politicians-make-a-difference-to-health-system-performance

Fact or fiction?
Comment series