Recent changes to commissioning and provider structures have left CCGs unsure about the future, and their GPs even less certain about what is expected of them.
CCGs were an attempt to pull clinicians into the process of commissioning. The model is designed to take into account a wide range of opinions. There should be clear lines of communication that in theory make it possible to trace the journey of every decision from the governing body right back to frontline GPs. Hospital doctors and nurses, practice nurses and other professionals also feed into this process.
The introduction of Sustainability and Transformation Plans and devolution agreements complicates this picture and takes decision-making further away from the frontline. To give an example: an average CCG in south west London has about 30 practices and operates alongside a coterminous health and wellbeing board and local authority. A Commissioning Collaborative now sits above this, spanning six CCGs and around 200 general practices. The Sustainability and Transformation Plan also takes place at this level and introduces into the process six local authorities and local acute, community and mental health trusts. At a higher level still, London has recently signed a devolution agreement which means that the region’s 1,400 practices (32 CCGs) will be working towards a vision to be negotiated with all 33 local authorities; the Mayor of London; NHS England; and Public Health England.
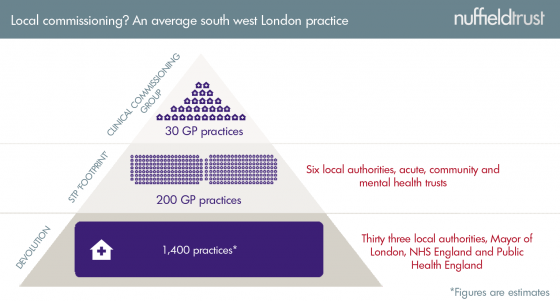
Potentially, this could all make sense: clearly there are some decisions that need to take place at a larger scale, particularly when it comes to specialist services or reorganisation plans. However, when their practice becomes just one of over one thousand practices, and their CCG just one of 32, do GPs still feel that they are in a system supposedly designed to “devolve power and responsibility for commissioning services to the healthcare professionals closest to patients”?
The clinical voice remains important to commissioning and there’s a simple explanation why. National leaders talk about the NHS being in serious need of transformational change, usually with significant implications for primary care. Ultimately the individuals who are going to enact these new ways of working are front line professionals. Without their input into what is needed, what would work and how patients might respond, willingness to actually implement these changes could be compromised. Clinical engagement, particularly by GPs, is often underestimated as a necessary factor in change but can be key a determinant of success. The structure of CCGs reflects this idea.
We’ve been exploring this issue with The King’s Fund for the last few years. Today’s report - Clinical commissioning. GPs in charge? - is the latest and final report of this programme, based on the learning of six CCGs. We review CCGs’ progress in strengthening the GP voice in commissioning, provide tips and recommendations for CCGs, NHS England and other national bodies on the future of the clinical voice in commissioning, and review the factors driving change in CCGs.
We find that CCGs have succeeded in making that voice heard in a number of ways. They have increased GP engagement in commissioning in comparison to previous forms, according to our research, and have taken advantage of the enthusiasm showed by some GPs in being more involved in how decisions are made. We asked GP leaders why they originally took on clinical commissioning roles, here’s what a few told us:
- ‘…I saw this as an opportunity to change things that affect my clinical life’
- ‘…I thought it’s a really exciting opportunity and I believed in it’
- ‘…to make real improvement on the ground’
And over the past few years, they have established themselves as an influential part of their local health economy. Their GP leaders feel increasingly confident in their roles.
How have CCGs achieved this? And how can we make sure these successes are retained even as the NHS changes?
Our research suggests that successful collaboration between CCGs and GPs is dependent on CCGs’ ability to retain local identity and build on collaborations that have evolved over time. This means being permissive to locally defined solutions rather than trying to force coalitions defined from above.
CCGs also need to be able to continue to harness enthusiasm among GPs to get involved in commissioning which will rest on having a persuasive offer to clinical leaders about the importance of their role in wider structures.
The result is that there are important considerations for NHS England and the Department of Health as the new commissioning and provider structures are established. We asked CCG leaders what message they would like to pass on to national leaders, and one told us “Allow CCGs to succeed before changing the structure”. That is advice worth listening to. We would add that national leaders should publish a vision for the future of commissioning that reflects the overlapping structures currently being developed across the country. And as a consequence of these new structures, there is a need for a clear statement reaffirming the principle of local clinicians (not just GPs) being at the heart of the commissioning process. Any further changes to the commissioning structure should be evolutionary, flexible to local conditions and importantly, should seek to retain some ‘localness’ in decision-making.
Without a commitment to listen to and act upon the clinical voice, we risk losing the progress made by CCGs in engaging local clinicians, and alienating those who feel that their efforts to participate have been in vain. Could these result in clinicians being less inclined to cooperate in the future? If so, current plans for service-level transformation might stall before they even really get started.
A version of this blog first appeared in the HSJ.
