This briefing explores the impact the pandemic has had on the delivery of rural and remote health services in England, highlighting the underlying challenges faced by these services – and outlining how the challenges faced are different for rural areas in comparison with more urban areas. It also discusses how performance could be monitored to signal the risk of any significant service pressures over the coming months.
Key points
- Rural and remote areas experienced problems that differentiate them from their more urban counterparts even before the Covid-19 pandemic. However, the pandemic has both exacerbated some of these challenges, as well as thrown up new ones.
- Covid-19 has had a more detrimental effect on hospital waiting times in rural and remote trusts than for trusts in more urban areas. In April 2020, the proportion of patients seen for their first consultant appointment for cancer fell by two-thirds (66%) in rural trusts compared with April 2019, whereas a decrease of 59% was seen in trusts located in more urban areas.
- Activity has fallen particularly dramatically in rural areas. Emergency admissions in April to June 2020 fell by 57% in rural trusts compared with the year before, while they fell by 45% elsewhere. The level of referral for talking therapies – via the Improving Access to Psychological Therapies (IAPT) programme – in rural areas was below half the level in April 2020 than it was a year before.
- The pandemic has exacerbated workforce issues in remote trusts. Remote trusts spend more on temporary staff (8% of their staffing budget) compared with other areas (6%). While the number of hospital and community health staff increased by 7% nationally in the year to June 2020, the workforce of remote trusts grew by only 5% over the same period.
- The underlying financial position of rural and remote services was worse than the position of more urban trusts before the pandemic started, and the pandemic may well have exacerbated this. Remote trusts’ debt was equivalent to more than half (56%) of their annual operating income in 2018/19. Remote trusts also typically do not seem to get their fair share of additional funding that goes into the NHS.
Context
The Covid-19 pandemic has repeatedly exposed the fault lines in the premise of a fair society and public services that are available to everyone. Health inequalities are a clear example, and for this paper we sought to explore briefly whether rural pressures might be another. There are many dimensions to the response of the NHS to the pandemic and the effect the pandemic has had on the service. For instance, initially across England there were efforts to free up hospital capacity to treat Covid-19 patients, which included increasing intensive care capacity, discharging patients and stopping elective care. Now services are seeking to address spiralling waiting lists for elective care.
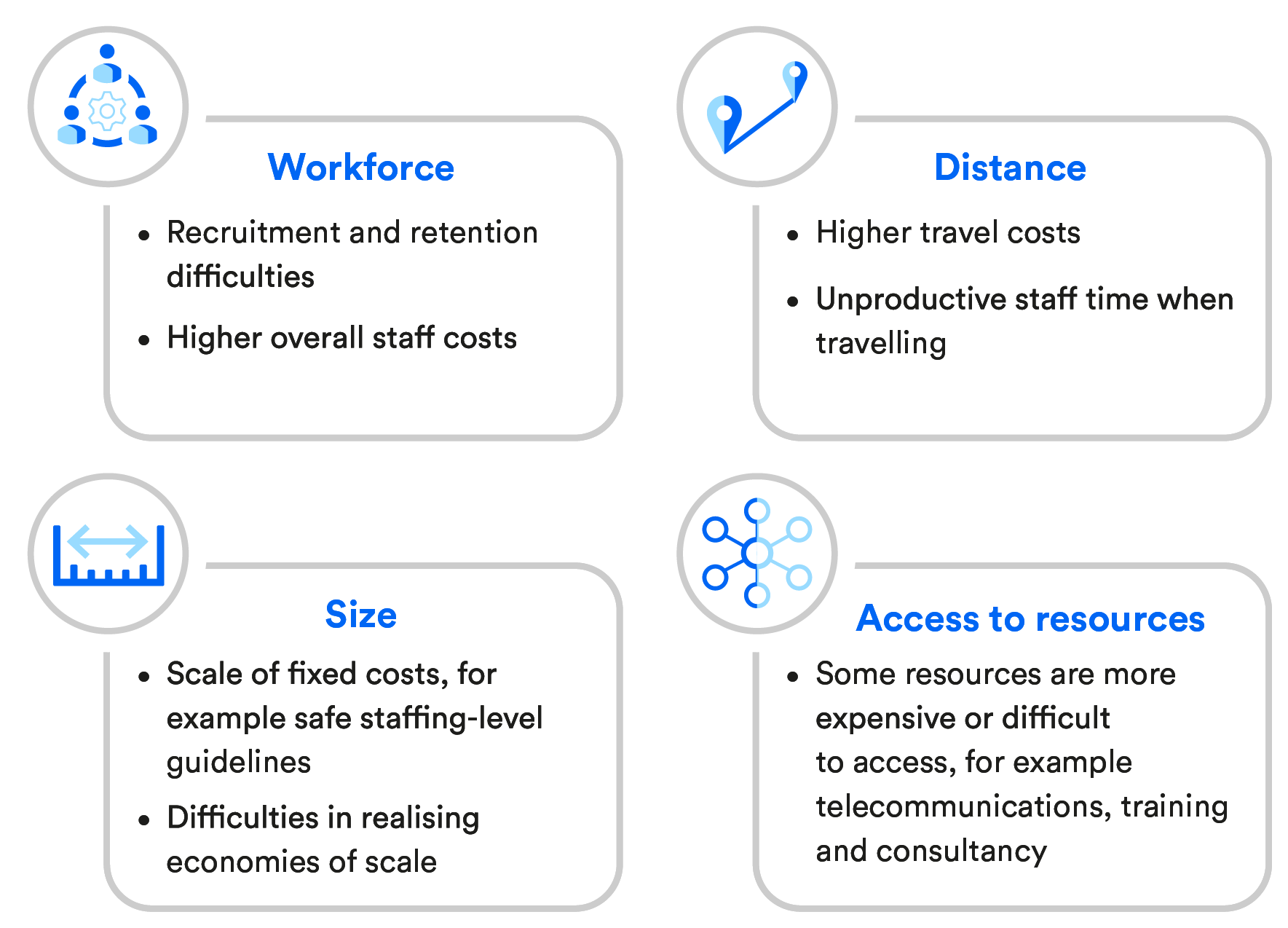
The challenges of providing care can vary in unavoidable or uncontrollable ways in different areas of England. It has long been recognised that rural and remote services have particular pressures, for a number of reasons, although quantifying the impact of these is challenging. If insufficient adjustment or compensation is made for the unavoidable costs involved, it is likely that some health services will not be able to afford to provide their population with the same access to, and quality of, care that others do. undefined
The pressures facing rural and remote health care services
This briefing explores the impact the pandemic has had on the delivery of rural and remote health services, highlighting some of the underlying challenges that services have faced and outlining how some of these are different in rural areas in comparison with more urban areas. We conclude with a discussion on how performance could be monitored to signal the risk of any significant service pressures over the coming months.
This was a short scoping exercise and not an exhaustive assessment. It is also primarily limited to NHS services, with a lack of readily available information on social care, making an assessment of the social care sector unfeasible. It is also important to note that non-urban trusts include a diverse range of providers, and while they face some similar challenges, they also have individual challenges. In this report we sought to look at rural and remote services separately.
For the purpose of our analysis, we defined rural trusts as the 10% with the highest proportion of patients admitted from rural areas, and clinical commissioning groups and local authorities were defined by Office for National Statistics’ 2011 rural–urban classification. Remote trusts are those considered to face higher costs due to their small size and location far from the next nearest service. For a list of the trusts defined as ‘rural’ and ‘remote’ for the purposes of this analysis, and for further details on our definitions, see Appendix A.
Health impact
Cases and deaths
Covid-19 has already had a direct impact on the health of many people. But the virus has a considerably higher health impact on older populations, which is significant for rural areas – 17% of the rural population of England are aged 70 and over, compared with 12% elsewhere. In the event, Covid-19 did not spread as early in rural areas as elsewhere: the peak of confirmed cases in non-rural areas (nearly one in 1,000 people in early April 2020) was evident about a month or so before the peak was seen in rural communities (which was around the same rate at the end of April). However, it remains unclear whether this trend is an artefact of the changing availability of testing.
As a result of the later spread to rural areas, mortality rates in these areas were initially lower than in urban centres: between March and May 2020, the age-and sex-standardised mortality rate from Covid-19 was highest in major urban conurbations (124 per 100,000 population), while rural towns and fringes saw a death rate of 59 per 100,000 population over the same period.
While the wider effect on public health is unclear, it is perhaps instructive to look at underlying influences, one of which is economic pressures. The most rural areas (those with more than 80% of the population living rurally) had the highest proportion of employees furloughed during both June and July 2020, at around two percentage points higher than in urban cities and towns (for example, 31% compared with 29% in the latter month).
Hospital waiting and ambulance response times
There are, of course, health effects not directly the result of Covid-19 but due to patients’ and services’ responses to the pandemic – such as delayed presentations and treatment. While the effect on patient outcomes is, as yet, unclear, the impact on waiting times and activity levels has been dramatic:
- From April to June 2020, with fewer patients presenting at Accident & Emergency (A&E), undefined the proportion of A&E patients seen within four hours (the waiting-time target) increased across all three geographies under study (rural, remote and all other areas). However, on average, A&E services still failed to hit the operational standard of 95%, with performance lower in remote trusts (91%) and rural providers (90%) compared with other trusts (93%).
- Since March 2020, hospital activity has dropped dramatically, with elective care postponed in many cases to release hospital capacity and many people apparently discouraged from using emergency services. By May 2020, elective activity had fallen by around two-thirds in rural and remote trusts – similar to that in all other trusts. However, rural trusts had a substantially greater fall in emergency admissions compared with all other providers. From April to June 2020, compared with the year before, emergency admissions fell by 57% in rural trusts, while they fell by 45% elsewhere.
- For cancer waiting times, in April 2020, rural and remote trusts fell short of achieving the target of 95% of their patients being seen within two weeks. As well as this, the number of patients actually being seen for their first cancer appointment with a consultant compared with the same time in 2019 reduced significantly (by 58% in remote areas and by two-thirds – 66% – in rural communities, compared with 59% in all other areas). However, over the same period, all trusts (including rural and remote) saw around a 25% decrease in the proportion of patients receiving their first cancer treatment within two months.
At the start of the pandemic, many ambulance trusts were already under immense pressure, with high rates of handovers to hospital emergency departments. Ambulance trusts tend to cover large areas, comprising big pockets of both urban and rural communities, making it difficult to unpick the particular effect of the pandemic on rural areas. However, the mean response time for Category 1 ambulance calls (those classified as life-threatening and requiring immediate intervention or resuscitation) over the past year in the Isle of Wight (the most sparsely populated area in England) was on average three-and-a-half minutes more than the England mean response time and on a par with the level seen during a large spike in March in London when it was a hotspot for Covid-19. undefined In cases where ambulance services were diverted to other centres, the impact on patients with coronavirus would have been substantial due to these patients being prone to rapid deterioration – potentially leading to poorer health outcomes. undefined
Mental health and social care
Given our reliance on existing data, much of this commentary focuses on general acute hospital services. However, there are indications that rural and remote services are facing challenges in other settings, including in terms of certain mental health and social care interventions.
Levels of referrals to Improving Access to Psychological Therapies (IAPT) services have decreased for all clinical commissioning groups but this has been more apparent among rural and remote providers. The number of referrals in April 2020 from rural clinical commissioning groups decreased by 52% from the year before, while all other clinical commissioning groups saw IAPT referrals decrease by 44%.
‘NHS continuing health care’ may be provided to some adults who have complex health needs. Historically, remote and rural areas have struggled with providing timely access to this care: between April and June 2017, more than a third (35%) of all referrals made in remote areas exceeded the target of 28 days; this compared with 23% in rural areas and 11% in more urban communities. However, by March 2020, the proportion of referrals exceeding 28 days dramatically decreased to, at most, 6% for these three geographical groupings, although overall, fewer referrals were being made.
Arguably, demand for care packages for vulnerable individuals during the pandemic would have increased, particularly in more rural areas where there are higher rates of older people. However, clinical commissioning groups were instructed to suspend continuing health care assessments during the Covid-19 peak, with these services resuming in September 2020. Given the high rates of delayed assessments in remote and rural areas pre-Covid, clinical commissioning groups and local authorities in these areas in particular may struggle to complete all retrospective and prospective assessments.
Funding
In April 2020, the government ‘wrote off’ the historic debt of NHS trusts, totalling £13.4 billion. The intention to intervene on debts was signalled before the pandemic but occurred during it. At the time, the level of debt for rural services – while large – was not, on average, dissimilar to debt for non-rural services – at around a sixth of annual operating income. However, the seven remote trusts had, on average, a far worse underlying financial position. Their debt in 2018/19 was, on average, equivalent to more than half (56%) of their operating income and accounted for a 10th (£1.3 billion) of their total debt, despite accounting for just 3% of their annual income. This again highlights the scale of financial challenges some remote services face.
There are many unavoidable reasons why these debts might have been accrued. When comparing like-for-like activity, the most remote hospital providers cost 8% more. Size can also matter; in primary care, one estimate suggests that a 10% increase in patient list size is associated with a 3% reduction in cost per patient. undefined , undefined Our previous work on health care in rural areas has highlighted some of the existing issues with allocations to rural areas, undefined which might also be causing them undue pressure (see the text box below).
Previous findings on allocations to rural areas
Our previous review of the current mechanisms for funding services, which includes the approach to allocating budgets to local commissioners and the payment system for NHS trusts, suggests the following:
- The weight given to adjustments for health inequalities and unmet need has a strong influence on allocations to rural areas. These adjustments are not informed by evidence, but remain a matter of judgement. This has the effect of directing the target allocations primarily towards urban areas.
- The scale of the adjustment for unavoidable smallness (£33 million in total) is very small compared with both other adjustments and NHS Improvement’s own calculation of unavoidable costs, which it used in adjusting the tariff for just one of the affected trusts (Morecambe Bay), which was equivalent to between £20 million and £25 million a year. In fact, subsequently published official documents suggest that around 80% of emergency care costs may be fixed. undefined
The actual allocations that specific areas receive are affected not only by population needs and unavoidable costs but also by historic funding levels. Policy-makers try not to destabilise local health economies by making large changes in funding. Overall, across the allocations for core, specialised and primary care services, this has the effect of moving money away from rural areas. undefined
History suggests that rural and remote services are at risk of not getting what might be deemed their fair share of the additional funding that is being injected into the NHS as a result of the pandemic. Much of the £32 billion that the Treasury has approved to support the health response to Covid-19 will be spent on national initiatives, but that will not account for all of it, with some being directed towards local services. However, looking back:
- the seven remote trusts received, in total, just 1.7% (£30 million out of £1,783 million) of the total allocation through the Sustainability and Transformation Fund in 2017/18 undefined
- similarly, the Provider Sustainability Fund, paid to trusts that accept their control totals* and deliver on both financial and operational performance, had the effect of reducing rural and remote trusts’ deficit by 0.7% and 0.3% respectively in 2018/19, compared with 1.6% for more urban trusts.
A lack of transparency about the flows of additional funding increases the risk that the funding is not distributed fairly and there is some evidence that rural services have been marginalised to some extent: for example, they have not received details about what equipment they might receive as a result of the pandemic as early as others. undefined
Capacity
Capacity to provide NHS care remains a key issue. Patients waiting more than a year for elective treatment grew exponentially from February to May 2020, undefined highlighting how trusts had to dramatically scale back their planned activity. Trusts have been told to return to near-normal levels of non-Covid services, delivering at least 80% of previous-year elective activity by September 2020, rising to 90% by October. undefined However, there remain questions – as outlined below – over the ability of rural and remote areas to provide sufficient capacity, through freeing up existing capacity, expanding capacity and using local non-NHS capacity to provide NHS care.
Nightingale hospitals
A key part of expanding capacity to cope with the pandemic was building a Nightingale hospital in seven locations across England (see the map below). Across all seven hospitals, there was the potential to provide up to 12,000 additional beds, albeit only two hospitals were used in the first wave of the pandemic, with no more than 200 patients being admitted. undefined However, these hospitals were very much an urban model and their location was not appropriate for patients in many rural areas. As one commentator has noted: ‘the centralisation of acute and/or intensive care services … makes much less sense for more rural and remote hospitals’. undefined As a second wave of infections takes hold, some of the Nightingale hospitals again appear to be part of the proposed solution to help manage demand, and so this remains a live issue for some rural areas.
Locations of the seven Nightingale hospitals

Independent sector
When the pandemic first hit the UK, independent providers played a pivotal role in extending services and facilities available to deal with the surge of Covid-19 patients. NHS England block-booked the equivalent of 8,000 beds and 20,000 clinical staff. undefined There is no readily accessible data on the distribution of independent sector capacity. However, data from 2016/17 suggested that, nationally, local commissioners spent £12 billion on purchasing health care from non-NHS providers – about £1 in every £6 they spent. Perhaps surprisingly, those commissioners from remote trusts spent more on the purchasing of health services from non-NHS bodies (20%) than their non-rural counterparts (16%), although in part this may be due to community interest companies playing a more significant role in community services in rural areas.
More recently, following concerns that the NHS would struggle to bring back near-normal levels of activity and waiting times, a contract notice stated that the NHS could spend up to £10 billion on outsourcing work to private providers over the next four years. undefined More work is needed to understand which areas have appropriate independent sector capacity to help clear rapidly increasing waiting lists for planned care.
Estates
In terms of trusts’ ability to increase capacity within their current estates, it is important to note that rural sites typically have less unoccupied floor space, so possibly less flexibility; 8% of floor space in non-rural sites is unoccupied compared with a lower level – just 5% – in rural areas. As well as this, before the pandemic struck, remote trusts had fewer occupied general and acute beds (77% occupied) compared with rural trusts (93%) and all other trusts (89%). That said, in the latest quarter (April to June 2020), data show large decreases in occupancy levels across England, which are particularly striking in rural services. These trusts may have felt pressure to discharge more patients to free up as much capacity as possible, particularly as they were unlikely to be able to benefit from the support of Nightingale hospitals.
Staffing
Another challenge is that of hospital staffing. We have previously highlighted that sparsely populated areas have greater difficulties in recruiting and retaining staff. undefined While there was a 7% national increase in staff in the year to June 2020, the workforce in remote trusts† grew at a slower rate over the same period (by 5%, compared with 8% for rural trusts). Remote trusts appear, for example, to have been less likely to benefit from students extending their clinical placements, since many of them are located further away from academic institutions. There is also a greater reliance on temporary staff to plug these gaps in remote areas. This comes at a significant cost, with 8% of remote trusts’ total spending on staff going towards bank and agency staff (compared with 5% in rural trusts and 6% elsewhere).
Building the workforce in primary care across England has been a struggle in recent years.‡ Over the period between June 2019 and June 2020, the available data suggest that while more urban areas saw a 0.7% (+145) increase in the number of full-time equivalent general practitioners (GPs), rural communities in fact experienced an increase of 1.1% (+124). This may reflect efforts of a targeted recruitment scheme in England, which is offering a financial incentive to GP trainees who commit to working in ‘hard to recruit’ areas, many of which are rural. undefined Despite this, previous analysis has found variation in the distribution of NHS dentists across England, with shortfalls being more apparent in rural and remote areas. undefined That said, the data for staff working in primary care is not complete nor comprehensive, with figures not including, for example, those employed by primary care networks. This needs to be rectified to provide appropriate assurance about the workforce.
Resilience
The uncertainty over NHS activity and the effect on capacity as a result of Covid-19 both to date and in the future is particularly problematic for rural and remote services. Generally speaking, rural and remote services are made up of smaller teams than those in urban services. Even small gaps in the workforce are felt more intensely if, for instance, sickness absence increases. Indeed, the latest data show that sickness absence this year increased to the highest levels ever seen in April – 2.1 percentage points higher than April 2019, and exceeding winter peaks of sickness absence recorded over the past 11 years. undefined
The limited availability of services in rural and remote areas also means that, were there to be any disruption to a particular provider, then the population might be left without an accessible alternative. For example, even within the current levels of provision, only 19% of the rural population are within 20 minutes’ walk of a community pharmacy, compared with 98% of the population in urban areas. undefined If such services were to close, it would further amplify these differences.
Rural and remote trusts are, by their nature, more likely to be isolated from other health care services. There are 19 small acute hospitals where more than half of the population would have to drive more than 30 minutes to the next nearest acute hospital. undefined These providers are therefore more compelled to provide a full array of services in a single estate.
As well as this, remote areas typically have a single, dominant provider, which they commission most services from. For example, five of the seven remote clinical commissioning groups have a single trust accounting for at least 80% of their spending, whereas this is the case in only half of non-rural clinical commissioning groups. There is a risk that reliance on a single hospital makes it much more challenging to reconfigure the space in response to Covid-19.
Conclusion and recommendations
That rural and remote providers experience problems that differentiate them from their urban counterparts is nothing new. However, the Covid-19 pandemic has both exposed these further and thrown up new challenges. It is imperative to tailor responses to the pandemic to take account of such differences, in order for teams to best assist the communities they serve. undefined Yet many national standards and policies were not appropriately adapted to meet the needs of rural areas even before the pandemic struck. undefined
Our work found that remote areas have specific workforce challenges, with the trend in workforce numbers failing to keep up with the national picture. We also discovered that remote commissioners tend to have one single, dominant provider that they commission most services from, potentially leaving them less resilient. In addition, rural trusts have less unoccupied floor space and could well be less likely to benefit from ambitions to use the urban-centric Nightingale model or the independent sector to clear waiting lists.
Additionally, long waiting times have historically been a greater problem for remote trusts, and we found that remote providers had greater drops in elective activity, longer waiting times and more delays in completing NHS continuing health care assessments compared with non-rural trusts during the period when Covid-19 was starting to take effect. Rural areas may feel greater pressure when trying to pick up normal care without the growing resources or capacity apparent in more urban areas.
This work was a short, exploratory exercise. Given the small number of remote organisations and the heterogeneous nature of the rural and non-rural groupings, the findings need to be treated with some caution.
However, there remain many important analytical avenues that could be pursued to better understand the relative challenges facing rural and remote services. In particular, these could include (but are not limited to):
- analysing the distance (drive times) that patients from different geographical areas are having to travel to access treatment
- exploring how the different types of geographies, such as coastal regions, might be particularly affected
- investigating suitable comparators to rural and remote services, such as comparing them only to those with similar characteristics (other than geography).
In terms of further work, we scoped a dashboard as part of this study, comprising a series of measures to track over time, relating to hospital activity and capacity, mental health care, primary care and social care (see Appendix B). Some of the data on these measures are included in the findings we have presented here and are also presented in Appendix B. The aim of such a dashboard is to help identify important service pressures and challenges facing rural and remote services. It also serves to highlight the pressures that rural and remote areas faced, both historically and at the brink of the Covid-19 pandemic.
Additional work should also seek to understand what particular mechanisms might be causing pressures in rural and remote services, such as the nature of the population they serve, capacity constraints or geographical characteristics. Given the importance of health services and the unique challenges that rural and remote services face, keeping a close eye on emerging pressures will be critical in these areas.
Other report resources:
View the dashboard [PDF]
Appendix A: Identifying rural and remote services [PDF]
Appendix B: Dashboard methodology and results [PDF]
About this briefing
In summer 2020, the National Centre for Rural Health and Care commissioned the Nuffield Trust to explore the challenges faced by rural areas in addressing the pandemic and asked that we explore what indicators could be used to continue to monitor this issue. The work builds on the report we were similarly commissioned to produce in 2019, entitled Rural health care: A rapid review of the impact of rurality on the costs of delivering health care.
Acknowledgements
We thank the National Centre for Rural Health and Care for funding and facilitating this study. In particular, we are grateful to Ivan Annibal, Professor Richard Parish and Jan Sobieraj for their input into the design of the work and ongoing support. We also thank the National Centre’s Board who provided useful comments on an earlier draft, as did our colleagues Rowan Dennison, Nigel Edwards and Dr Louella Vaughan.
Partners

Suggested citation
Palmer W and Rolewicz L (2020) Rural, remote and at risk: Why rural health services face a steep climb to recovery from Covid-19. Report, Nuffield Trust.

